Full text
Background
The coronavirus disease 2019 (COVID-19) pandemic resulted in the temporary closure of many population-based cancer screening programs worldwide1, including BreastScreen NSW, which was temporarily paused for 7 weeks in 2020 in response to safety considerations. From June 2021, BreastScreen NSW again suspended services in the state of New South Wales (NSW) due to the increasing incidence of the COVID-19 Delta strain and the need to redeploy staff to support the pandemic response. While services have reopened, there is concern among clinicians and public health professionals internationally about the potential adverse impacts of service suspensions on breast cancer morbidity and mortality, and a call for shared learnings on best practice for the resumption of services.1 This retrospective observational study aimed to examine data before and after the 2020 BreastScreen NSW suspension to assess the impact on tumour size in breast cancer diagnoses, and volumes of mastectomy and breast-conserving surgery.
Methods
Two analyses were conducted on retrospective data contained in NSW Health administrative datasets: 1) the NSW BreastScreen Information System (BIS) which records all service information for screeners and cancer diagnoses; and 2) the NSW Cancer Registry (NSWCR) which contains population-based data on cancer stage, treatment and care (including surgery notifications).
Analysis 1: delayed screening
The first analysis selected all women aged 50–74 years who attended a BreastScreen NSW service and were diagnosed with invasive breast cancers. The distributions of tumour sizes were examined for two comparisons:
- Clients with and without a delay in screening (due to the service suspension) for the year following the service suspension (1 June 2020–31 May 2021); and
- Clients with a delay in screening before and after the suspension (1 March 2019–29 February 2020 and 1 June 2020–31 May 2021).
The closure period of 1 March 2020 to 31 May 2020 was chosen to allow for the staggered reopening of breast screening services across NSW. In line with the National Accreditation Standards (NAS) measures of BreastScreen Australia, patients who attended their rescreening appointment after 27 months for biennial screeners, or 15 months for annual screeners, were classified as “delayed”.2 For the first comparison, any screening services that had already been delayed before the service suspension were excluded because these delays might not be directly attributable to the suspension. The second comparison did not exclude clients whose rescreen had already been delayed before the service suspension. Distributions of tumour sizes were compared using both the t-test and the Kolmogorov–Smirnov (K-S) test.
Analysis 2: breast surgery
The second analysis included all women aged 50–74 years who underwent surgery for both screen- and non-screen-detected breast cancers. The analysis used cancer surgery notification data from the NSWCR to compute volumes of breast-conserving surgery and breast mastectomies from 2018 to 2020. Expected counts for the period 1 March 2020–31 December 2020 were based on matched monthly counts for the preceding period of 1 January 2018–29 February 2020. Three-year time series of 36 monthly totals of surgery in public and private facilities were examined with exponentially weighted moving average (EWMA) charts.
Data were analysed using SAS 7.1 and R 4.0.2 packages (tidyverse & QCC).3,4
The NSW Population and Health Services Research Ethics Committee assessed the study as not raising any ethical risks requiring submission to an ethical review body in accordance with NSW Health Policy (Quality Improvement and Ethical Review GL2007_020).
Results
In the year following the suspension of services (1 June 2020 to 31 May 2021) there were 2079 incident cancers among women who had previously screened with BreastScreen NSW. Of the 2079, 409 were diagnosed from a delayed service due to the suspension of BreastScreen NSW services; 1315 were diagnosed from a non-delayed service; and 355 were excluded from the analyses due to the screening being delayed prior to the service suspension.
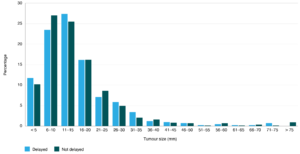
The mean tumour size for delayed women was 16.2 mm (median 13.0 mm; 25th percentile 8.0 mm; 75th percentile 20.0 mm) compared to 15.9 mm (median 12.0 mm; 25th percentile 8.0 mm; 75th percentile 22.0 mm) for women who were not delayed (Figure 1). No significant difference was found in the tumour size between groups (p-value 0.6748; t-test; K-S p-value 0.7216).
Figure 1. Distributions of tumour size of diagnosed cancers in the BreastScreen NSW service after suspension, for both delayed and non-delayed screeners between 1 June 2020 and 31 May 2021. (click figure to enlarge)
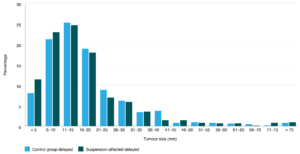
For the second comparison, between 1 March 2019 to 29 February 2020, there were 644 incident cancers found in clients whose screening had been delayed (control group). This is in comparison to 764 cancers detected from 1 June 2020 to 31 May 2021 in the suspension-affected group.
The mean tumour size for the suspension-affected group was 17.2 mm (median 14.0 mm; 25th percentile 8.8 mm; 75th percentile 20.0 mm) compared to 18.0 mm (median 15.0 mm; 25th percentile 10.0 mm; 75th percentile 22.0 mm) for clients in the control group (Figure 2). No significant difference was found in mean tumour size between groups (p-value 0.2813; t-test. K-S p-value 0.3230).
Figure 2: Distributions of tumour sizes of diagnosed cancers for the control group (before services were suspended: 1 Mar 2019 to 29 Feb 2020) and the suspension-affected group (after services were suspended: 1 June 2020 to 31 May 2021). (click figure to enlarge)
Figure 3 shows the monthly breast-conserving and mastectomy surgery from 1 January 2018 to 31 December 2020. The volume of breast conserving surgeries declined by approximately half during and shortly after the 2020 service suspension period. Over the period 1 March 2020–31 December 2020, there were 340 fewer (–15%) breast-conserving surgeries than expected based on the comparison period. The change in volume of mastectomies observed was smaller, with only 50 fewer (–7%) mastectomies than expected based on the comparison period. Volumes of breast conserving surgery and mastectomies returned to typical monthly caseloads by September. EWMA charts confirmed evidence of an interruption in breast-conserving surgery in both public and private facilities, with a lesser impact on mastectomies.
Figure 3. Three-year time series of monthly breast cancer activity in NSW public and private facilities (click figure to enlarge)
Discussion & conclusions
Our retrospective analyses demonstrated no evidence of a substantial change in the size of tumours diagnosed by BreastScreen NSW in clients whose breast cancer screening was delayed by the suspension of service due to the COVID-19 pandemic, relative to clients who screened on-time. The analysis found no increase in tumour size following the 2020 suspension of service, relative to the tumour size seen in the years prior to the suspension of service. The analysis also showed that while breast-conserving surgery volumes in NSW hospitals decreased following the suspension of services in early-mid 2020, levels recovered to typical caseloads by September 2020.
Our findings are comparable to that seen in national and international literature.1,5-8 Cancer Council Australia’s microsimulation modelling examined the potential COVID-19 impacts on BreastScreen Australia-wide and reported only small stage shifts with small increases in tumour size. For example, the proportion of population-level invasive cancers that are small (≤ 15 mm) was estimated to be 54% for a 3-month pause, or 48% for a 12-month pause.7 International research has reported that short-term interruptions of cancer screening may not result in cancers of more advanced stage being diagnosed, particularly when screening services catch up with any backlogs quickly.5,8
Findings in this report may not be reflective of other Australian states and territories due to variations in COVID-19 restrictions. For example, the state of Victoria had longer and tighter restrictions than NSW, and an analysis has demonstrated significant reductions in breast cancer notifications.9 Long-term monitoring and evaluation of the impact of COVID-19 and subsequent disruptions on BreastScreen NSW, including the impact on breast surgery volumes, cancer staging, and survival outcomes, are warranted.6
The study findings should be considered in light of several limitations. Firstly, additional factors that can affect the tumour size at diagnosis including screening annually or biennially, screeners’ age, and use of hormone replacement therapy, should be investigated in further analyses. Secondly, BreastScreen NSW has not recorded any noticeable increases in self-reported shifts to private screening. It is possible that larger tumours resulting from delayed screening have been diagnosed symptomatically, rather than through scheduled asymptomatic screening. If this has occurred, it will become evident in an increased rate of interval cancers. While this will be detected through normal quality assurance monitoring, proactive analysis of linked data from BreastScreen NSW screening and the NSWCR should be undertaken to confirm or refute this hypothesis when complete NSWCR data for the study period become available. Given that the impact of COVID-19 on BreastScreen NSW is likely to be complex, this data linkage will allow a more comprehensive investigation of the dynamics of breast cancer screening and cancer incidence. Thirdly, this study has only included data relating to the 2020 BreastScreen NSW service closure. The Cancer Institute NSW is continuing to analyse the impact of the 2021 service closure.
The results of this study highlight the importance of quantifying the impacts of the COVID-19 pandemic on population-based cancer screening programs, to inform evidence-based policy decision making and the development of targeted pandemic recovery strategies.1 The findings enabled Cancer Institute NSW to provide reassurance to the public that the benefits of the suspension of screening (redeployment of BreastScreen NSW staff to the pandemic response and reduction of infection risk) was likely to outweigh any potential harms such as increase in tumour size and increased invasiveness of breast cancer treatments.
Peer review and provenance
Externally peer reviewed, not commissioned.
Copyright:
© 2022 Jayakody et al. This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International Licence, which allows others to redistribute, adapt and share this work non-commercially provided they attribute the work and any adapted version of it is distributed under the same Creative Commons licence terms.
References
- 1. Alkatout I, Biebl M, Momenimovahed Z, Giovannucci E, Hadavandsiri F, Salehiniya H, et al. Has COVID-19 affected cancer screening programs? A systematic review. Front Oncol. 2021;11:675038. CrossRef | PubMed
- 2. Australian Institute of Health and Welfare 2019. BreastScreen Australia data dictionary: version 1.2. Canberra: AIHW; 2019 [cited 2022 Jul 5]. Available from: Available from: www.aihw.gov.au/reports/cancer-screening/breastscreen-australia-data-dictionary-version-1-2/summary
- 3. SAS Institute Inc. SAS/ACCESS 9.4 Interface to ADABAS: Cary, NC: SAS Institute Inc; 2013.
- 4. R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2020. Available from: www.R-project.org/
- 5. Eijkelboom AH, de Munck L, Lobbes MBI, van Gils CH, Wesseling J, Westenend PJ, et al. Impact of the suspension and restart of the Dutch breast cancer screening program on breast cancer incidence and stage during the COVID-19 pandemic. Prev Med. 2021;151:106602. CrossRef | PubMed
- 6. Eijkelboom AH, de Munck L, Vrancken Peeters M, Broeders MJM, Strobbe LJA, Bos M, et al. Impact of the COVID-19 pandemic on diagnosis, stage, and initial treatment of breast cancer in the Netherlands: a population-based study. J Hematol Oncol. 2021;14(1):64. CrossRef | PubMed
- 7. Nickson C Procopio P, Deij S, Velentzis L. COVID-19 scenario modelling for cancer screening programs, the BreastScreen Australia Program, May 2020. Cancer Council NSW, Cancer Research Division [cited 2021 Nov 1]. Available from: www.health.gov.au/sites/default/files/documents/2020/09/covid-19-scenario-modelling-for-cancer-screening-programs-the-breastscreen-australia-program.pdf
- 8. Yin K, Singh P, Drohan B, Hughes KS. Breast imaging, breast surgery, and cancer genetics in the age of COVID-19. Cancer. 2020;126(20):4466–72. CrossRef | PubMed
- 9. Te Marvelde L, Wolfe R, McArthur G, Blake LA, Evans SM. Decline in cancer pathology notifications during the 2020 COVID-19-related restrictions in Victoria. Med J Aust. 2021;214(6):281–3. CrossRef | PubMed