Abstract
Objective: Gaps and complexities exist in cancer referral and diagnosis in Australia, leading to delays in cancer treatments. Developing evidence-based referral pathways is important for promoting better and more timely cancer diagnosis and care.
Type of program or service: This paper describes a toolkit endorsed by the Cancer Institute NSW as a guide for promoting best practice in localising cancer referral and diagnosis pathways in line with the national Optimal Care Pathways.
Use of toolkit: Employing methods in the toolkit yielded an increased understanding of cancer care pathways, strengthened collaboration between tertiary and primary sector stakeholders, and enhanced the project skills of Cancer System Innovation Managers. The toolkit has become a valuable guide for consolidating referral pathways for various cancers in the NSW local health districts and could apply to cancer services in other jurisdictions.
Lessons learnt: The pilot project showed that the toolkit is useful in developing referral pathways and reflects best stakeholder engagement practices. Local evidence should be generated to support systematic change and should include the perspectives of cancer patients and clinicians. NSW local health districts continue to use the toolkit methods to optimise care to improve outcomes for people living with cancer.
Full text
Cancer care pathways toolkit: what it is and how it can help
Pathways to cancer diagnosis and treatment have long been identified as problematic. Delayed or inappropriate referrals from primary care to specialist services remain a significant issue in cancer care and can result in delayed diagnosis and poor patient experience.1-4 Since 2015, the Cancer Institute NSW (the Institute) has been supporting the development of a common approach to localising referral pathways in cancer services in New South Wales (NSW), Australia. Local pathways for people living with cancer should align with the national Optimal Care Pathways frameworks5 to reduce complexities and variabilities associated with cancer diagnosis and referral.2,6-8 Facilitated by the Research in Implementation Science and eHealth (RISe) group, University of Sydney, the pilot project initially focused on pathway development for the diagnosis and referral of lung cancer. A pathways implementation framework was developed and piloted in two local health districts (LHDs) in NSW, with outcomes from the pilot informing the creation of a mapping and dissemination toolkit.9 The pilot sites collaborated with other NSW LHDs within a lung cancer pathway Community of Practice to deliver a toolkit that could be implemented across the state of NSW. This paper aims to briefly describe the toolkit and highlight strategies focused on localising referral pathways to reduce variation in cancer diagnosis and treatment, which is a priority for the Institute.
Toolkit characteristics and functions
The toolkit, endorsed by the Institute, is a practical guide for health professionals involved in developing and disseminating localised pathways for cancer diagnosis and referral.9 Localising a pathway refers to overlaying local services and referral points onto the Optimal Care Pathways – frameworks outlining the best cancer care for specific cancer types.5 Localisation of pathways fosters common understanding and transparency of the critical points and recommended health professionals involved along the pathway, promoting quality evidence-based cancer care and positive patient experiences. Understanding the critical points in the pathway can provide a benchmark for evaluation and monitoring that aim to reduce variation in care and promote timely diagnosis.6,7
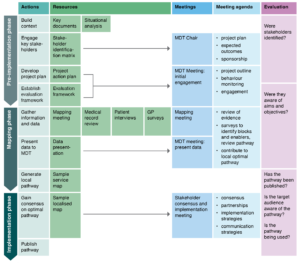
Local health districts are encouraged to utilise the toolkit for priority cancers, focusing on quality improvement and patient safety. Key stakeholders involved in the localisation activities and processes are Cancer System Innovation Managers (CSIMs), multidisciplinary team members (MDTs), service managers, clinical leads, and clinicians in primary health care. The toolkit9 consists of four sections: 1) identification and analysis of needs; 2) pre-implementation project formulation; 3) pathway mapping; and 4) dissemination, monitoring and evaluation. These implementation processes and associated activities are described in Figure 1. Dissemination of the localised pathways includes promotion through primary health networks (PHNs) and other primary care-focused activities such as general practitioner (GP) meetings, workshops and professional development programs. They are then further developed and disseminated through web-based platforms, such as HealthPathways.10
Figure 1. Project cycle for mapping and localising cancer referral and diagnosis pathways (click figure to enlarge)
GP – general practitioners; MDT – multidisciplinary team.
Source: Cancer Institute NSW. Cancer care pathways: mapping and dissemination toolkit. Sydney: Cancer Institute NSW; 20229
Toolkit pilot and evaluation
In 2015, the RISe group worked with the CSIMs in South Western Sydney LHD (SWSLHD) and Northern NSW LHD (NNSWLHD) to pilot the toolkit. NNSWLHD undertook pilot activities across the district. At SWSLHD, the toolkit was piloted with the district Lung Cancer MDT members hosted at Liverpool Hospital, which included clinicians from Liverpool, Bankstown and Macarthur treatment centres. The evaluation involved monitoring the experience and outcomes of mapping and developing lung cancer care pathways in the two LHDs. Four CSIMs completed a 10-item pilot evaluation questionnaire, rating items on a five-point scale from highly agree (scored as 5) to highly disagree (scored as 1). The three highest-rated items were: ‘the toolkit content to be relevant for the purposes of the current project’ (75% highly agreed), ‘the information in the toolkit is practical and useful’ (75% highly agreed) and ‘I believe the toolkit will be relevant generally across all LHDs’ (50% highly agreed; 50% agreed). Participants gave lower ratings to two items which were that the tools and appendices needed some further improvement and the usefulness of illustrations, figures, tables and web-links. In qualitative feedback, one CSIM thought the graphic displays needed further refinements to include links to GP guides and weblink updates. These concerns were addressed before the toolkit was finalised.
Both sites reported being given the opportunity to participate in toolkit review and felt that their feedback was acknowledged and incorporated. The pilot sites had positive experiences using the toolkit resources, and participating CSIMs believed that the pathway mapping process resulted in significant progress in local stakeholder engagement and increased their understanding of lung cancer pathways within the LHDs. The quarterly Community of Practice meetings, which included CSIMs from non-pilot sites, enabled CSIMs to collaborate and improve project skills. The project team observed increased engagement between tertiary and primary sectors, including PHN, GP and LHD stakeholders. Both pilot sites achieved consensus on a local pathway for their LHD and confirmed that they reflected best practices whilst acknowledging the care needs of local populations.
The pilot sites reported that engagement with peers was beneficial as it provided opportunities to share challenges and solutions regarding project management, data access, conducting a medical record review, and methods of engagement with project stakeholders. The participation of primary care stakeholders at the mapping and consensus meetings was fundamental to ensuring that the pathway was comprehensive. Early engagement with the primary care sector and ongoing involvement of a GP liaison and HealthPathways representative was reported as largely advantageous to developing and disseminating the pathway. The pilot sites adopted varying methods of primary sector engagement, including information sessions with primary care professionals. Early and consistent clinician engagement was key to clarifying the current local pathways and making changes where required. Survey responses highlighted that respiratory physicians acted as project champions to lead change. A consistent and active presence of respiratory physicians in the Lung Cancer MDT meetings was critical to the implementation and success of all project components.
A significant barrier, however, was the time required to complete the project, including the time to publish and evaluate the local pathways. Feedback from the CSIMs at the pilot sites suggested possible challenges with ethics and governance approvals for the implementation activities. It is recommended that team members consider early in the process if ethics and governance are needed for the project, for example, if patient interviews will be undertaken.
Current reflections
The two pilot sites, represented by authors SA and SM, continue to benefit from skills developed in the pilot and to use the toolkit to implement local cancer referral pathways. The pilot project demonstrated that diagnostic delays were a compelling reason to clarify and improve local referral pathways. For example, SWSLHD established a rapid access lung cancer clinic and ‘Referral Decision Prompt’ reporting tool for imaging services that see people with suspicious lesions, and offer referral guidance for GPs.11 In NNSWLHD, the skills gained through the initial project expedited future pathway localisation by leveraging existing knowledge and stakeholder relationships. To improve the timeliness of future projects, both SWSLHD and NNSWLHD submitted an ethics application to cover subsequent referral pathways being developed.
Service mapping remains valuable in identifying key stakeholders across multiple organisations that can provide input or utilise the pathways as intended. Patient audits and interviews still provide important information to identify the current referral pathways and whether they are understandable and lead to appropriate referrals. Pathways should continue to be made available through an accessible and integrated platform, such as HealthPathways, as this helps clinicians use them across the health system.
Early and structured engagement with GPs, PHNs and specialist clinicians remains key to the successful development and implementation of new local referral pathways. If all stakeholders are not engaged in the process, it can be difficult to reset referral patterns based on evolving evidence within established professional networks. Evaluating and maintaining current local referral pathways can be challenging, as it requires dedicated resourcing across partners.
Lessons learnt
Fragmented cancer care pathways are a recurring problem, particularly in the context of multiple service providers and professionals involved in delivering care.1-4,6 The Institute continues to support connections between primary and tertiary settings, with LHDs continuing to use the cancer care pathways toolkit to optimise care to improve outcomes for people living with cancer. This toolkit is a pragmatic and evidence-based resource, aligned with the national Optimal Care Pathways frameworks5, that supports the development of cohesive and local referral pathways to reduce variation in cancer care. In this way, the toolkit may also be useful for cancer services in other jurisdictions to localise referral pathways.
Acknowledgements
The authors would like to acknowledge Cancer Institute NSW which funded the original pilot project used to develop the toolkit. We are also grateful to the T3 Flagship program in lung cancer, Sydney Catalyst Translational Cancer Research Centre (TCRC), University of Sydney and Cancer Australia’s Lung Cancer Demonstration Project, which have significantly informed the development of the toolkit resource. The authors would also like to acknowledge Cancer System Innovation Managers across NSW who were involved in the original Community of Practice meetings.
Peer review and provenance
Externally peer reviewed, not commissioned.
Copyright:
© 2023 Norsa et al. This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International Licence, which allows others to redistribute, adapt and share this work non-commercially provided they attribute the work and any adapted version of it is distributed under the same Creative Commons licence terms.
References
- 1. Qu LG, Nzenza T, McMillan K, Sengupta S. Delays in prostate cancer care within a hospital network in Victoria, Australia. ANZ J Surg. 2019;89(12):1599–604. CrossRef | PubMed
- 2. Otty Z, Brown A, Sabesan S, Evans R, Larkins S. Optimal care pathways for people with lung cancer-a scoping review of the literature. Int J Integr Care. 2020;20(3). CrossRef | PubMed
- 3. Malalasekera A, Dhillon HM, Blinman PL, Kao SC, Vardy JL. Delays to diagnosis and treatment of lung cancer in Australia: healthcare professional perceptions of actual versus acceptable timeframes. Intern Med J. 2018;48(9):1063–71. CrossRef | PubMed
- 4. Purdie S, Creighton N, White KM, Baker D, Ewald D, Lee CK, et al. Pathways to diagnosis of non-small cell lung cancer: a descriptive cohort study. NPJ Prim Care Respir Med. 2019;29(1):1–6. CrossRef | PubMed
- 5. Cancer Council. Optimal care pathways. Sydney: Cancer Council Australia; 2021 [cited 2022 Feb 23]. Available from: Available from: www.cancer.org.au/health-professionals/optimal-cancer-care-pathways
- 6. Bergin RJ, Thomas RJ, Whitfield K, White V. Concordance between Optimal Care Pathways and colorectal cancer care: Identifying opportunities to improve quality and reduce disparities. J Eval Clin Pract. 2020;26(3):918–26. CrossRef | PubMed
- 7. Rankin NM, York S, Stone E, Barnes D, McGregor D, Lai M, et al. Pathways to lung cancer diagnosis: a qualitative study of patients and general practitioners about diagnostic and pretreatment intervals. Ann Am Thorac Soc. 2017;14(5):742–53. CrossRef | PubMed
- 8. Te Marvelde L, McNair P, Whitfield K, Autier P, Boyle P, Sullivan R, et al. Alignment with indices of a care pathway is associated with improved survival: an observational population-based study in colon cancer patients. EClinicalMedicine. 2019;15:42–50. CrossRef | PubMed
- 9. Cancer Institute NSW. Cancer care pathways: mapping and dissemination toolkit. Sydney: Cancer Institute NSW; 2022 [cited 2022 Feb 23]. Available from: www.cancer.nsw.gov.au/about-cancer/document-library/cancer-care-pathways-mapping-and-dissemination-too
- 10. HealthPathways. About HealthPathways. New Zealand: HealthPathways; 2021 [cited 2022 Feb 23]. Available from: healthpathwaysglobal.org/About
- 11. Rankin N, York S, Trevena L, Emery J, Sundaresan P, Beale P, Shaw T. P3. 13-038 The RoaDmaP Study: feasibility of implementing a primary care intervention for referral of potential lung cancer cases to specialist care. J Thorac Oncol. 2017;12(11):S2329–S30. CrossRef