Abstract
Objective: There have been no trials in healthcare settings of genetic susceptibility feedback in relation to alcohol consumption. The purpose of this study was to determine the feasibility and acceptability of conducting a full-scale randomised trial estimating the effect of personalised genetic susceptibility feedback on alcohol consumption in hospital outpatients with risky drinking.
Methods: Outpatients ≥18 years of age who reported drinking more than 14 standard drinks in the past week or in a typical week were asked to provide a saliva sample for genetic testing. Genetic susceptibility feedback was posted to participants 6 months after recruitment. The co-primary outcomes were the proportion of participants who (i) provided a saliva sample that could be genotyped, and (ii) spoke with a genetic counsellor. Secondary outcomes included changes in patients’ weekly alcohol consumption; scores on scales measuring readiness to change, importance of changing and confidence in ability to change drinking habits; knowledge about which cancers are alcohol-attributable; and acceptability of the saliva collection procedure and the genetic-feedback intervention. McNemar’s test and paired t-tests were used to test for differences between baseline and follow-up in proportions and means, respectively.
Results: Of 100 participants who provided a saliva sample, 93 had adequate DNA for at least one genotyping assay. Three participants spoke to a genetic counsellor. Patients’ readiness to change their drinking, their views on the importance of changing and their stated confidence in their ability to change increased between baseline and follow-up. There was no increase in patients’ knowledge about alcohol-attributable cancers nor any reduction in how much alcohol they drank 4 months after receiving the feedback. Most participants (80%) were somewhat comfortable or very comfortable with the process used to collect saliva, 84% understood the genetic feedback, 54% found it useful, 10% had sought support to reduce their drinking after receiving the feedback, and 37% reported that the feedback would affect how much they drink in the future.
Conclusion: Results of this study suggest it would be feasible to conduct a methodologically robust trial estimating the effect of genetic susceptibility feedback on alcohol consumption in hospital outpatients with risky drinking.
Full text
Introduction
Consumption of alcohol is causally related to cancer of the oral cavity and pharynx, larynx, oesophagus and upper aerodigestive tract, colorectum, liver and female breast.1 Alcohol-attributable cancer caused 337 400 deaths globally in 2010, or 4.9 deaths per 100 000 people.2 The mechanisms by which alcohol consumption increases the risk of cancer are not fully understood, but a genotoxic effect of acetaldehyde from alcohol metabolism in the body has been identified as a likely causal pathway for several alcohol-related cancers.1 Given the “relationship between alcohol consumption and cancer is monotonic and without threshold”,1 Cancer Council Australia recommends that people limit their drinking to reduce their risk of cancer, and advises individuals who choose to drink alcohol to do so in accordance with the National Health and Medical Research Council (NHMRC) guidelines for reducing the lifetime risk of harm from alcohol consumption.3,4
One in five Australians is a risky drinker.5 To reduce alcohol consumption, the World Health Organization recommends the delivery of alcohol screening and brief intervention in the primary health care setting.6 This strategy is modestly effective, with reductions in consumption of 13% lasting 12 months among nontreatment-seeking patients with risky drinking.7 Personalised medicine, defined as “the application of genetic information to predict disease development, influence decisions about lifestyle choices, and tailor preventative intervention or medical treatment to the individual needs of each patient”8, might be more effective than screening and brief intervention because of its personal salience.9 Although the findings from a recent systematic review do not support this hypothesis, only four studies met the criteria for a low summary risk of bias and none of these evaluated the effect of genetic feedback on alcohol consumption in healthcare settings.10
The purpose of this study was to determine the feasibility of conducting a full-scale randomised trial estimating the effect of personalised genetic susceptibility feedback on alcohol consumption in hospital outpatients with risky drinking. This setting was chosen because one in three hospital outpatients report risky drinking11, compared with one in four primary care patients12 and one in five Australian adults.5 We have previously reported that people recruited in the proposed outpatient setting are reluctant to leave their seat for fear of missing their appointment, illustrating the importance of thorough piloting of experimental procedures.13 Accordingly, one of this study’s primary outcomes was the feasibility of collecting saliva samples that could be genotyped. Previous research has shown that the provision of genetic susceptibility results by mail with telephone follow-up for counselling is as effective as in-person counselling14, but some recent studies have relied on mail alone.15,16 Therefore, this study’s other primary outcome was whether participants expressed the need for genetic counselling by telephone after the provision of genetic susceptibility results by mail.
Methods
This feasibility study was conducted in the outpatient department (Ambulatory Care Centre) of a large public hospital in Newcastle, Australia, which provides services for more than 870 000 people residing in a region the size of England.17
Ethical approval for this study was obtained from the Hunter New England Human Research Ethics Committee (13/11/20/4.09) and the University of Newcastle Human Research Ethics Committee (H-2014-0203).
Eligibility, recruitment and screening
Outpatients ≥18 years of age who were capable of completing the screening questionnaire on an iPad, and who reported drinking more than 14 standard drinks in the past week or in a typical week were eligible. We approached potential participants in the waiting area and logged consenting outpatients into the screening questionnaire on an iPad using a unique identifier. Page 1 briefly described the Alcohol Genetic Risk Information Project. Page 2 collected demographic data (gender, age and postcode). Page 3 asked respondents if they had consumed alcohol in the past 12 months (yes or no). Those who had not were excluded at this point. Page 4 comprised a 7-day retrospective drinking diary, and page 5 asked participants to select the number of standard drinks they consumed in a typical week: 1–7, 8–14, 15–21, 22–28, 29–35, 36–42, 43–49, 50–56, 55–63, 64–70 and 71+.
Participants who reported consuming ≤14 standard drinks in the past week and ≤14 standard drinks in a typical week were excluded at this point. Page 6 asked participants questions about their readiness to change their drinking habits, the importance of changing their drinking habits and their confidence in their ability to change their drinking habits.18 Page 7 assessed participants’ knowledge about alcohol-attributable cancers.
Saliva collection
Saliva was collected using a whole-saliva collection device – the Oragene DNA (OG-500) self-collection kit – which has been shown to provide a significantly greater DNA yield than the cytobrush, foam swab and oral rinse methods.19 Participants are required to spit until the saliva reaches the fill line (2 mL). Participants had the option of providing the saliva sample in the waiting area, one of the nearby rest rooms, or in the consulting room immediately before or after their appointment.
Genotyping assays
DNA samples were genotyped with TaqMan® single nucleotide polymorphism genotyping assays. The choice of assays was based on evidence of increased cancer risk because of altered enzyme activity (increased production of acetaldehyde), as well as the frequency of the risk allele in Caucasians.
The ADH1B*2, ADH1C*1 and ADH7*2 alleles increase acetaldehyde production through increased enzyme activity of 40-, 2.5- and 100-fold, respectively.20 Caucasians have a 50% ADH1C*1 allele (rs1693482) frequency and a 10% ADH*2 allele (rs1573496) frequency.20 The ADH1B*1 allele (rs1229984) was also included, because this allele is associated with head and neck cancer in epidemiological studies and has almost 100% allele frequency in Caucasians.21
Intervention
Personalised behavioural and genetic susceptibility feedback was posted to participants 6 months after recruitment (Figure 1). The expressed need for genetic counselling by telephone after the provision of genetic susceptibility results by mail was assessed by randomly allocating participants to receive one of:
- A letter enclosed with their feedback encouraging them to call the research team to organise a telephone appointment with a genetic counsellor
- A telephone call from the research team shortly after their feedback had been posted.
During the telephone call, participants received a brief explanation of the feedback and were offered a telephone appointment with a genetic counsellor. Participants were also asked how they felt about getting their results in the post, whether it was useful to have someone call to explain the results, and if they thought it might be necessary for participants to have a face-to-face meeting with a genetic counsellor.
Figure 1. Example of personalised behavioural and genetic feedback
Follow-up
Four months after the genetic susceptibility feedback had been posted, we sent participants a letter on university stationery (with a $20 supermarket voucher redeemable irrespective of further participation) advising them they would receive a follow-up questionnaire in the next few days. Participants who provided an email address were sent a message embedded with a unique hyperlink to the follow-up questionnaire, and the remainder were sent a paper copy. Reminders were sent at 2-week intervals. The first was sent by email or post as per the initial contact, and the second by post because offering different response modes sequentially (web then post) has been shown to improve response rates.22 After a further 2 weeks, telephone follow-up was attempted and participants were invited to complete the questionnaire by telephone when contact was made.
Primary outcomes
Feasibility of collecting saliva samples that can be genotyped
The feasibility of collecting saliva samples was measured as the proportion of eligible consenting outpatients who reported consuming >14 standard drinks in the past week or in a typical week, and who provided a saliva sample that could be genotyped.
Expressed need for telephone counselling
The expressed need for genetic counselling by telephone after the provision of genetic susceptibility results by mail was measured as the proportion of participants with a saliva sample that could be genotyped and who spoke with a genetic counsellor.
Secondary outcomes
Weekly alcohol consumption
A 7-day retrospective diary was used to measure the volume of alcohol consumed in the past week.23
Readiness to change, importance of changing and confidence in ability to change drinking habits
Visual analogue scales ranging from 1 to 100 were used to measure participants’ readiness to change, importance of changing and confidence in ability to change drinking habits. The questions were:18
- How ready are you to change your drinking habits?
- How important is it for you right now to change your drinking?
- If you decide to change your drinking habits, how confident are you that you would succeed?
Knowledge
Participants were asked “Which of the following cancers is related to a person’s alcohol consumption?” The response options were ‘no’, ‘yes’, and ‘don’t know’ for each of the following cancers: bladder, breast, colon and rectal, mouth and throat, kidney, liver, lung, ovarian, pancreatic, and prostate.
Acceptability
Participants were asked:
- How comfortable did you feel when providing the saliva sample? (very comfortable, somewhat comfortable, somewhat uncomfortable, very uncomfortable)
- Did you understand the genetic risk information? (no, yes)
- Did you find the genetic risk information useful? (very useful, quite useful, somewhat useful, not useful at all)
- Have you sought support to reduce your drinking as a consequence of receiving the genetic risk information? (no, yes)
- Will the genetic risk information affect how much you drink in the future? (no, yes)
Survey on attitudes to genetic susceptibility testing
We briefly surveyed outpatients’ attitudes to genetic susceptibility testing. We told participants that “Some genes put people at a higher risk of developing an alcohol-related cancer. The test for these genes involves providing a saliva sample”. We then asked them “If you could be tested for these genes while waiting for your appointment here today, would you want to get the test done?” After participants had provided a yes or no response, they were asked to provide one or more reasons for their decision.
Data analyses
Data were analysed using Stata 11.1 (StataCorp, College Station, TX, US). Descriptive statistics (frequencies and percentages for discrete variables, and medians with interquartile ranges for continuous variables) were used to summarise participants’ characteristics at baseline (gender, age, alcohol consumption). McNemar’s test and paired t-tests were used to test for differences between baseline and follow-up in proportions and means, respectively.
Results
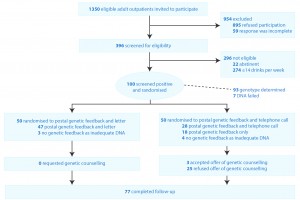
Of the 1350 outpatients invited to participate, 895 (66%) refused and 59 (4.4%) did not complete the screening process because they were called for their appointment. Of the 396 participants who completed the screening questions, 296 (75%) were excluded – 274 (69%) reported drinking ≤14 drinks in the past week or in a typical week, and 22 (5.6%) reported not drinking any alcohol in the past year. Of the 100 (25%) who reported drinking >14 standard drinks in the past week or in a typical week, 87 were male, their mean age was 45.7 years (standard deviation17.4), and the median (25th and 75th percentile) number of standard drinks they consumed was 22 (17, 32). Most participants (77/100) completed the follow-up questionnaire (Figure 2). There were no significant differences between participants observed and unobserved at follow-up with regard to gender, age and number of standard drinks consumed in the past week or in a typical week at baseline.
Figure 2. Recruitment, enrolment and retention
Primary outcomes
Feasibility of collecting saliva samples that can be genotyped
Of the 100 saliva samples collected, 93 contained adequate DNA for at least one genotyping assay.
Expressed need for telephone counselling
Of the 93 participants who provided adequate DNA for at least one genotyping assay, 47 were allocated to the letter arm of the study and 46 were allocated to the telephone arm. None of the participants allocated to the letter arm called to organise an appointment with a genetic counsellor. We were unable to offer 18 of the 46 participants allocated to the telephone arm an appointment with a genetic counsellor because:
- Nine did not answer any of our calls
- Six said we had called at an inconvenient time and failed to answer when we called back at the nominated suitable time
- Three advised us that they were no longer interested in participating (one person was in hospital, one was “beyond the age of worrying” and one gave no reason).
Three of the 28 participants we contacted chose to speak with a genetic counsellor. One participant declined because he didn’t have time (59-year-old man) but most felt it was not needed – for example:
I don’t really need it. I know and I understand. (61-year-old woman)
Don’t have a need for that. (25-year-old man)
All of the participants we spoke to felt postal feedback was acceptable – for example:
Nice to have a hard copy. Time to think about it and digest. Or email. (55-year-old man)
Some participants found the follow-up telephone call helpful – for example:
I didn’t realise that about the gene so thank you that’s very helpful to get a call. (48-year-old man)
Some found it useful from a confirmatory point of view – for example:
Put my mind at ease that I read it right. (71-year-old woman)
Others thought it was unnecessary – for example:
Someone might not understand, but I had no problem understanding. (35-year-old man)
Most participants did not express the need for a face-to-face meeting with a genetic counsellor, but thought others might – for example:
Some people maybe. (44-year-old man)
Depends on the person. (64-year-old man)
I wouldn’t personally want that. (66-year-old man)
Secondary outcomes
Weekly alcohol consumption
The volume of alcohol consumed in the past week did not decrease between baseline and follow-up (Table 1).
Readiness to change, importance of changing and confidence in ability to change drinking habits
Participants’ scores on scales measuring readiness to change, importance of changing and confidence in ability to change drinking habits increased between baseline and follow-up (Table 1).
Table 1. Change in weekly alcohol consumption and psychological constructs between baseline and follow-up among retained participantsa
| Measure (range) | Baseline median (25th, 75th percentiles) | Follow-up median (25th, 75th percentiles) | Mean change | 95% confidence interval | p valueb |
| Number of standard drinks consumed in the past week | 21 (17, 31) | 21 (15, 34) | –0.29 | –4.26, 3.69 | 0.89 |
| Readiness to change drinking habits (1–100) | 21 (0, 45) | 25.5 (5, 58) | 9.43 | 3.26, 15.61 | <0.01 |
| Importance of changing drinking habits (1–100) | 16 (0, 48) | 26 (7.5, 70.5) | 10.82 | 3.93, 17.70 | <0.01 |
| Confidence in ability to change drinking habits (1–100) | 54 (23, 80) | 68 (38, 90) | 8.92 | 0.96, 16.89 | 0.03 |
a Seventy-seven participants completed both questionnaires
b Statistical significance was determined by paired t-tests
Knowledge
There was no increase in the proportion of participants who correctly identified which cancers are related to alcohol consumption and which are not between baseline and follow-up.
Acceptability
Participants’ responses to questions about acceptability are shown in Table 2. Positive feedback provided in the comments section of the follow-up questionnaire included:
It has made me rethink my drinking problem and act on fixing it. (48-year-old man)
It has made me stop drinking; I only drink about every 1–2 months. (52-year-old woman)
Some of the less positive feedback provided in the comments section included:
Thought this would be good, but it’s a waste of time. Did it because I thought I would get an idea of risk of cancer but didn’t tell me anything. Don’t know if I’m at risk of colon cancer or specific details, just an increased risk from drinking alcohol. (45-year-old man)
I didn’t read it very carefully. Off-hand I don’t think it was a very good result. And I prefer not to know the risks. (48-year-old man)
Table 2. Findings regarding acceptability among retained participantsa
| Questions | Available answers | n (%) |
| How comfortable did you feel when providing the saliva sample? | Very comfortable
Somewhat comfortable Somewhat uncomfortable Very uncomfortable |
35 (46)
26 (34) 9 (12) 6 (7.9) |
| Did you understand the genetic risk information? | No
Yes |
12 (16)
63 (84) |
| Did you find the genetic risk information useful? | Very useful
Quite useful Somewhat useful Not useful at all |
12 (16)
28 (38) 25 (34) 9 (12) |
| Have you sought support to reduce your drinking as a consequence of receiving the genetic risk information? | No
Yes |
66 (90)
7 (10) |
| Will the genetic risk information affect how much you drink in the future? | No
Yes |
44 (63)
26 (37) |
a Seventy-seven participants responded at follow-up
Survey on attitudes to genetic susceptibility testing
Of the 100/138 (73%) outpatients who consented, 26/100 (26%) said they would not agree to have the genetic susceptibility testing. The reasons given were no or low alcohol use (14 participants), no family history of cancer (5 participants), worry about result (4 participants), inconvenience of test (3 participants), concerns about privacy (2 participants), not worried about cancer (1 participant) and too old (1 participant).
Discussion
This study suggests that it would be feasible to conduct a methodologically robust trial estimating the efficacy of genetic susceptibility feedback in hospital outpatients with risky drinking, despite the three main problems we encountered.
First, the consent rate was low. This would inflate the cost of a trial by increasing the time required to recruit enough participants for adequate study power. The low consent rate may also reduce the generalisability (external validity) of effect estimates. The findings of this study facilitate the design of a trial with high internal validity by increasing the duration of recruitment. Given that approximately 500 people attend outpatient appointments at the Ambulatory Care Centre each day, we estimate it would take 12 months to recruit the required number of people in this setting.
Second, 7% of saliva samples obtained using the Oragene DNA (OG-500) collection system did not contain adequate DNA because the participants were unable to produce the required 2 mL of saliva. The oral rinse method, which involves swishing vigorously with 10 mL of mouthwash for 45 seconds before expectorating the mouthwash into a clean specimen cup, provides high-quality DNA, but it requires immediate processing, which is not practical.19 Another option is the use of DNA from blood, but this is invasive and likely to be inconvenient, because participants would need to visit the pathology collection centre before leaving the hospital. Given that the Oragene DNA (OG-500) self-collection system remains the best option, outpatients would be eligible for inclusion in a trial only if their saliva sample can be genotyped. This approach may reduce the generalisability of the effect estimates, but it would preserve internal validity, which must be the priority in an efficacy trial.24
Third, we were unable to contact many of the participants by telephone. It should be noted that:
- Only 3 of the 28 participants we contacted chose to speak with a genetic counsellor
- The other participants declined because they understood the feedback
- No-one in the group allocated to receive a letter encouraging them to call the research team to organise a telephone appointment with a genetic counsellor did so.
These results suggest that genetic counselling by telephone after the provision of genetic susceptibility results by mail is not needed. Since expressed need may underestimate actual need, it may be prudent to provide participants in a trial with the option of speaking to a genetic counsellor.
There was no reduction in alcohol consumption between baseline and follow-up. This is not surprising, because the study was not powered to detect a clinically meaningful change in alcohol consumption. The finding that patients’ readiness to change their drinking, their views on the importance of changing, and their stated confidence in their ability to change increased between baseline and follow-up is encouraging, given that high readiness, high importance and high confidence have been shown to predict reductions in alcohol consumption.18,25 Participants’ knowledge as to which cancers were alcohol-attributable did not increase after receiving information about these associations. This arguably suggests that the focus of public health messages should be on the alcohol–cancer link per se, rather than on specific cancers. There may be value in undertaking interviews with participants to investigate how they process this information and what would help increase retention.
Limitations
The study was not powered to detect a clinically meaningful change in alcohol consumption. Furthermore, the lack of a control group prevents inferring a relationship between the intervention and any changes in drinking. The purpose of the study was to examine the acceptability of the intervention to the target population of patients, and to gather data that would inform a decision about the feasibility of a large, robust efficacy trial, and the design of such a trial.
Conclusion
Results of this study suggest it would be feasible to conduct a methodologically robust trial estimating the efficacy of genetic susceptibility feedback in hospital outpatients with risky drinking. If efficacy is shown, there is a high potential for health benefits, but if the intervention is found to be ineffective, policy makers and the health research community will have valuable information about where not to invest scarce resources.26
Acknowledgements
This project was funded by a grant from the Mental Health and Drug and Alcohol Office (MHDAO), NSW Ministry of Health, LMB 961 North Sydney NSW 2059. KK is supported by an NHMRC Senior Research Fellowship (APP1041867). Neither the MHDAO nor NHMRC had a further role in the study design; in the collection, analysis and interpretation of the data; in the writing of the report; or the decision to submit the paper for publication. We thank the Hunter New England Local Health District, and the manager of the Ambulatory Care Centre in particular, for facilitating the research; and the outpatients who participated in this study.
Copyright:
© 2016 Johnson et al. This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International Licence, which allows others to redistribute, adapt and share this work non-commercially provided they attribute the work and any adapted version of it is distributed under the same Creative Commons licence terms.
References
- 1. IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Personal habits and indoor combustions. Volume 100 E. A review of human carcinogens. IARC Monogr Eval Carcinog Risks Hum. 2012;100(Pt E):1–538. PubMed
- 2. Rehm J, Shield KD. Global alcohol-attributable deaths from cancer, liver cirrhosis, and injury in 2010. Alcohol Res. 2013;35(2):174–83. PubMed
- 3. Winstanley MH, Pratt IS, Chapman K, Griffin HJ, Croager EJ, Olver IN, et al. Alcohol and cancer: a position statement from Cancer Council Australia. Med J Aust. 2011;194(9):479–82. PubMed
- 4. National Health and Medical Research Council. Australian guidelines to reduce health risks from drinking alcohol. Canberra: NHMRC; 2009 [cited 2016 Apr 1]. Available from: www.nhmrc.gov.au/_files_nhmrc/publications/attachments/ds10-alcohol.pdf
- 5. Australian Institute of Health and Welfare. 2010 National drug strategy household survey report. Canberra: AIHW; 2011 [cited 2016 Apr 1]. Available from: www.aihw.gov.au/WorkArea/DownloadAsset.aspx?id=10737421314&libID=10737421314
- 6. World Health Organization. Global status report on noncommunicable diseases 2014. Geneva: WHO; 2014 [cited 2016 Apr 1]. Available from: www.who.int/nmh/publications/ncd-status-report-2014/en/
- 7. Kaner EF, Beyer F, Dickinson HO, Pienaar E, Campbell F, Schlesinger C, et al. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst Rev. 2007;18(2):CD004148. CrossRef | PubMed
- 8. National Health and Medical Research Council. Clinical utility of personalised medicine. Canberra: NHMRC; 2011 [cited 2016 Apr 1]. Available from: www.nhmrc.gov.au/_files_nhmrc/publications/attachments/ps0001_clinical_utility_personalised_medicine_feb_2011.pdf
- 9. McBride CM, Koehly LM, Sanderson SC, Kaphingst KA. The behavioral response to personalized genetic information: will genetic risk profiles motivate individuals and families to choose more healthful behaviors? Annu Rev Public Health. 2010;31:89–103. CrossRef | PubMed
- 10. Hollands GJ, French DP, Griffin SJ, Prevost AT, Sutton S, King S, Marteau TM. The impact of communicating genetic risks of disease on risk-reducing health behaviour: systematic review with meta-analysis. BMJ. 2016;352:i1102. CrossRef | PubMed
- 11. Johnson NA, Kypri K, Latter J, McElduff P, Saunders JB, Saitz R, et al. Prevalence of unhealthy alcohol use in hospital outpatients. Drug Alcohol Depend. 2014;144:270–3. CrossRef | PubMed
- 12. Britt H, Miller GC, Henderson J, Charles J, Valenti L, Harrison C, et al. A decade of Australian general practice activity 2003–04 to 2012–13. Canberra: Sydney University Press; 2013 [cited 2016 Apr 1]. Available from: ses.library.usyd.edu.au//bitstream/2123/9366/8/9781743323793_ONLINE.pdf
- 13. Johnson NA, Kypri K, Attia J. Development of an electronic alcohol screening and brief intervention program for hospital outpatients with unhealthy alcohol use. JMIR Research Protocols. 2013;2(2):e36. CrossRef | PubMed
- 14. McBride CM, Halabi S, Bepler G, Lyna P, McIntyre L, Lipkus I, et al. Maximizing the motivational impact of feedback of lung cancer susceptibility on smokers' desire to quit. J Health Commun. 2000;5(3):229–41. CrossRef | PubMed
- 15. Godino JG, van Sluijs EM, Marteau TM, Sutton S, Sharp SJ, Griffin SJ. Effect of communicating genetic and phenotypic risk for type 2 diabetes in combination with lifestyle advice on objectively measured physical activity: protocol of a randomised controlled trial. BMC Public Health. 2012;12:444. CrossRef | PubMed
- 16. Meisel SF, Beeken RJ, van Jaarsveld CH, Wardle J. Genetic susceptibility testing and readiness to control weight: results from a randomized controlled trial. Obesity (Silver Spring). 2015;23(2):305–12. CrossRef | PubMed
- 17. NSW Health. Hunter New England. Sydney: NSW Ministry of Health; [cited 2016 Apr 1]. Available from: www.health.nsw.gov.au/lhd/pages/hnelhd.aspx
- 18. Bertholet N, Horton NJ, Saitz R. Improvements in readiness to change and drinking in primary care patients with unhealthy alcohol use: a prospective study. BMC Public Health. 2009;9:101. CrossRef | PubMed
- 19. Rogers NL, Cole SA, Lan H-C, Crossa A, Demerath EW. New saliva DNA collection method compared to buccal cell collection techniques for epidemiological studies. Am J Hum Biol. 2007;19(3):319–26. CrossRef | PubMed
- 20. Druesne-Pecollo N, Tehard B, Mallet Y, Gerber M, Norat T, Hercberg S, et al. Alcohol and genetic polymorphisms: effect on risk of alcohol-related cancer. Lancet Oncol. 2009;10(2):173–80. CrossRef
- 21. Osier MV, Pakstis AJ, Soodyall H, Comas D, Goldman D, Odunsi A, et al. A global perspective on genetic variation at the ADH genes reveals unusual patterns of linkage disequilibrium and diversity. Am J Hum Genet. 2002;71(1):84–99. CrossRef | PubMed
- 22. Millar M, Dillman D. Improving response to web and mixed-mode surveys. Public Opin Q. 2011;75:249–69. CrossRef
- 23. Gmel G, Rehm J. Measuring alcohol consumption. Contemp Drug Probl. 2004;31:467–540.
- 24. Rothman KJ, Greenland S, Lash TL. Modern Epidemiology. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkin; c2008. 758p.
- 25. Bertholet N, Gaume J, Faouzi M, Gmel G, Daeppen JB. Predictive value of readiness, importance, and confidence in ability to change drinking and smoking. BMC Public Health. 2012;12:708. CrossRef | PubMed
- 26. Chalmers I, Bracken MB, Djulbegovic B, Garattini S, Grant J, Gülmezoglu AM, et al. How to increase value and reduce waste when research priorities are set. Lancet 2014;383(9912):156–65. CrossRef | PubMed