Abstract
Objective: To pilot surveillance to describe environmental, personal and behavioural risk factors for people presenting to hospital emergency departments (EDs) with heat illness.
Methods: We conducted a retrospective case series and telephone interview study of people presenting to EDs across South Western Sydney, Western Sydney and Nepean Blue Mountains Local Health Districts with heat illness over the 2017/18 and 2018/19 summer periods (1 December to 28 February). We used the Public Health Rapid Emergency Disease Syndromic Surveillance (PHREDSS) ‘heat problems’ syndrome to identify people with heat illness and medical records to find contact details. We developed a detailed questionnaire instrument to guide the telephone interview.
Results: A total of 129 individuals presented with ‘heat problems’ (57 in 2017/18 and 72 in 2018/19). The median age was 44 years (range 1–89 years). Most attended hospitals via the NSW Ambulance Service (58%) or private car (40%). Of the total, 53% were classified as triage category 3 (potentially life-threatening), 27% as category 4 (potentially serious) and 16% as category 2 (imminently life-threatening). The main supplementary codes were heat exhaustion (35%), heat syncope (39%), and heat stroke (30%). The majority were discharged from the emergency department after completing treatment (73%), with 21% requiring admission. A total of 38 follow-up interviews were completed (29% response rate). Almost all individuals were exposed to heat outside their home environment: 11 (29%) were engaged in paid work, 5 (13%) in outdoor housework, and 10 (26%) in outdoor recreational activities.
Conclusion: Our pilot surveillance study successfully collected home, local environment and behavioural risk factors on a small cohort presenting with ‘heat problems’ to EDs in Western Sydney during the summer months. Most were exposed to heat outdoors while engaged in work or recreation outside the home, and were preventable.
Full text
Introduction
Classical epidemiological methods using interviews or questionnaires to obtain details of risk factors, such as case-control studies, have seldom been used to study heat illness because they are more resource-intensive and rely on identifying cases of heat-related illness or death.1-4 However, there is potential for these methods to yield rich and locally relevant information to assist with tailoring public health messages, understanding adaption priorities and prevention advice, and enabling follow-up action. In contrast, time series epidemiological studies based on routine data sources are excellent for quantifying cause-specific morbidity and mortality burden and are less resource intensive, but do not identify specific persons presenting with a condition caused by heat and lack detailed person-based, residential, and environmental information that allows us to identify specific vulnerabilities.5-7 The ongoing collection of risk information from cases of heat-related illness through case-based surveillance and follow-up interviews could be an important method to enhance our understanding of the causes of heat-related illness.
Personal risk factors associated with heat illness include cardiovascular5, renal5, respiratory disease6, psychiatric illness8, ethnicity9, mobility3, and social isolation.3,4 Behavioural factors include dressing;, personal cooling2; physical activity levels10; and attention to news or warnings. Environmental risk factors include dwelling type, location on a top floor2, and having a working air conditioner4,11or fans. There is less epidemiological evidence for the importance of eaves, blinds, roof colour, shade, and green surrounds.12,13The relevance and importance of the above factors may vary depending on local circumstances. Most of these factors can only be obtained through interviews and/or site inspections.
We chose to study heat-related presentations in Western Sydney, home to approximately 2.5 million people and hotter than the eastern parts of the city because it is deprived of the temperature moderation provided by the sea and sea breezes.14
This study aimed to pilot a collection of information that could form a future case-based surveillance system to provide ongoing intelligence about people who present with heat-related conditions.
Methods
We conducted a retrospective case series and interview study of presentations to public hospital emergency departments (EDs) with ‘heat problems’. Participants presented to 14 EDs across South Western Sydney, Western Sydney and Nepean Blue Mountains Local Health Districts (LHDs) with a heat-related illness over the 2017/18 and 2018/19 summer periods (1 December to 28 February).
Data on ED presentations with an ED diagnosis of ‘heat problems’ were obtained from the Public Health Rapid Emergency Disease and Syndromic Surveillance (PHREDSS) system which monitors several syndromes of public health importance through ED electronic records.15 ‘Heat problems’ is an umbrella term used in the Systematised Nomenclature of Medicines –Clinical Terminology (SNOMED-CT) nomenclature that includes heat exhaustion, heat stroke, heat syncope, heat cramps, and anhidrotic heat exhaustion.16 The following variables were obtained from PHREDSS for each presentation: medical record number, arrival date, diagnosis code, diagnosis description, patient ID, age in years, sex, arrival mode, departure status, triage category, hospital name and postcode. Research collaborators at each LHD accessed participants’ electronic medical records using the patient identifier from the record obtained from PHREDSS. Contact details for participants were obtained from the electronic medical record (name, contact phone number, address, next of kin and next of kin phone number).
A detailed questionnaire instrument (see supplementary File 1, doi.org/10.6084/m9.figshare.24558301) was developed largely following the work of Zhang et al.4 and Naughton et al.11 The interview instrument asked about: demographic information health status including any medical conditions4; functional ability17; perceived social supports18; access to transport; living conditions and building features, as well as information on the participant’s activity and location, and awareness of heatwave warnings prior to the heat illness presentation.
Authors KA or SG conducted a telephone interview with consenting participants who presented to EDs with heat problems during the 2017/18 and 2018/19 summer periods. For presentations of children and adolescents interviews were conducted with their parent or guardian. As per ethics approval, consent to complete the telephone interview was obtained at the initial telephone call with an option to be posted a participant information sheet and be recontacted by telephone or decline. Interviews with people presenting to emergency in summer 2017/18 were delayed until late 2018. After an ethics amendment, data collection was extended to the summer of 2018/19. In early 2019, we received data weekly from PHREDSS and interviews were attempted closer to the time of the ED presentation. PHREDSS data and interview data were recorded on a Microsoft Excel spreadsheet and analysed in the program.19 Data was stored on a password-protected network drive.
Bureau of Meteorology (BoM) data was accessed to prepare figures showing the relationship between daily ‘heat problem’ presentations and daily maximum temperatures averaged from three representative monitoring stations in Western Sydney. We used simple univariable Poisson regression in Stata20, with maximum daily temperature as the exposure and ‘heat problem’ presentations per day as the outcome to describe the association. This study was approved by the South Western Sydney Local Health District Human Research Ethics Committee (HREC/18/LPOOL/219).
Results
There were 129 presentations for ‘heat problems’ over the two summer periods in the three LHDs. The association with daily maximum temperature is shown in Figures 1 and 2. For each degree increase in maximum daily temperature, there was a 20% increase in the likelihood of an emergency department presentation with ‘heat problems’ (combined summers).
Figure 1. Daily presentations to Western Sydney emergency departments with ‘heat problems’: 1 December 2017 to 28 February 2018 (click figure to enlarge)
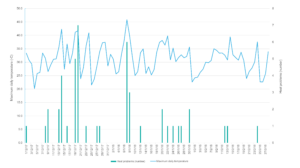
Figure 1. Daily presentations to Western Sydney emergency departments with ‘heat problems’: 1December 2017 to 28 February 2018
Figure 2. Daily presentations to Western Sydney emergency departments with ‘heat problems’: 1 December 2018 to 28 February 2019 (click figure to enlarge)
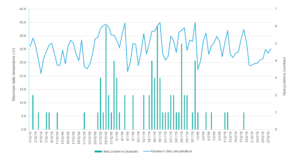
Figure 2. Daily presentations to Western Sydney emergency departments with heat problems: 1 December 2018 to 28 February 2019
There were 57 individuals who presented with ‘heat problems’ in 2017/18 and 72 in 2018/19. The 129 individuals with ‘heat problems’ had a median age of 44 years (range 1-89 years). Most attended hospitals via the NSW Ambulance Service (58%) or private car (40%). More than half (53%) were in triage category 3 (potentially life-threatening), 27% in category 4 (potentially serious), 16% in category 2 (imminently life-threatening) and 3% in category 1 (immediate attention). The main supplementary diagnostic codes were: heat exhaustion (35%), heat syncope (39%) and heat stroke (30%). The majority were able to be discharged from the ED after assessment and completing treatment (73%), with 20% requiring admission (Table 1).
Table 1. Summary characteristics of 129 emergency department presentations with ‘heat problems’ over two summers, and subset of 38 interviewees
| Characteristic | ED presentations (N =129) n (%) |
Interview subset (N = 38) n (%) |
| Summer period 2017/18 | 57 (44) | 11 (29) |
| Summer period 2018/19 | 72 (56) | 27 (71) |
| Diagnosis description frequency | ||
| Heat exhaustion | 45 (35) | 16 (42) |
| Heat stroke | 30 (23) | 8 (21) |
| Heat syncope | 39 (30) | 13 (34) |
| Heat cramps | 5 (4) | 1 (3%) |
| Other | 10 (8) | 0 |
| Median age, [range (years)] | 44 [range 1–89] | 46 [range 6–89] |
| Sex | ||
| Male | 88 (68) | 21 (55) |
| Female | 41 (32) | 17 (45) |
| Arrival mode | ||
| Ambulance | 75 (58) | 21 (55) |
| Private car | 51 (40) | 16 (42) |
| Invalid | 3 (2) | 1 (3) |
| Triage category | ||
| 1 (immediate attention) | 4 (3) | 0 (0) |
| 2 (imminently life-threatening) | 21 (16) | 5 (13) |
| 3 (potentially life-threatening) | 69 (53) | 26 (68) |
| 4 (potentially serious) | 35 (27) | 7 (18) |
| 5 (less urgent) | 0 (0) | 0 (0) |
| Mode of leave | ||
| Admitted to critical care | 1 (1) | 0 (0) |
| Admitted to ward | 26 (20) | 7 (18) |
| Transferred | 1 (1) | 1 (3) |
| Departed, treatment completed | 94 (73) | 30 (79) |
| Did not wait//left at own risk/missing | 7 (5) | 0 (0) |
Of the 129 cases with heat problems, 38 interviews were completed (response rate 29%). Eleven interviews were conducted for the 2017/18 summer (19% response rate) and 27 for the 18/19 summer (response rate 38%). For 22 cases, the phone was out of service or call restricted, eight declined an interview, one had died (not due to heat-illness), and for 60 presentations, there was no response to the attempted telephone contact.
Demographic and social factors of the people interviewed are summarised in Table 2. The median age of the interviewees was 46 years (range 6–89 years). Twenty-one were male (55%). Median family income was in the $60 000–90 000 range, 21 had completed Year 12 or above in their education (55%). Overall, they had good health. The main medical comorbidity was hypertension. Functionally, almost all interviewees were independent. Most reported receiving visits from friends or neighbours, but a number reported ‘never having visits from friends or neighbours (n = 11, 28%). Most believed they received understanding from others and could count on others for help if required. Most lived in detached brick houses constructed in the last 30 years, and the majority had access to air conditioning. (Table 2).
Table 2. Selected personal, social and environmental factors of interviewees (N = 38)
| Characteristic | |
| Age, median (range), years | 46 (6–89) |
| Male n, (%) | 21 (55%) |
| Median annual income category ($) | $60-90,000 |
| University qualification n, (%) | 5 (13%) |
| Underlying medical conditiona n, (%) | 13 (34%) |
| Language spoken at home | |
| English n, (%) | 33 (87) |
| Other n, (%) | 5 (13) |
| Social connection | |
| Receive visits from friends/neighbours n, (%) Never Less than once a week, More than once a week |
11 (29) 12 (32) 15 (39) |
| Partake in social activities n, (%) Never Less than once a week More than once a week |
5 (17) 12 (32) 21 (55) |
| Living alone n, (%) | 3 (8) |
| Dwelling type | |
| House n, (%) | 31 (82) |
| Apartment n, (%) | 5 (13) |
| Terrace/townhouse n, (%) | 2 (5) |
| Construction – brick n, (%) | 22 (58) |
| Dwelling age >30 years n, (%) | 12 (38) |
| Dark coloured roof n, (%) | 22 (58) |
| Air conditioning n, (%) | 33 (87) |
| Fans n, (%) | 27 (71) |
| Home comfort rating in hot weather (>35°C)b | |
| Hot n, (%) | 9 (24) |
| Warm n, (%) | 9 (24) |
| Slightly warm n, (%) | 5 (13) |
| Neutral n, (%) | 15 (39) |
a Heart disease (n = 2), respiratory disease(n = 2), asthma (n = 1), kidney disease (n = 2), hypertension (n = 13), diabetes (n = 1), depression (n = 3), cancer (n = 3).
b Home comfort rating as reported by participants.
Almost all interviewees were exposed to heat outside their home environment (Table 3). Nearly one-third were engaging in paid work (n = 11, 29%), which included manual labour such as landscaping, moving homes and raising scaffolding. Of this group, five were aware of work-related policies relating to protection from heat. A further group (n = 5, 13%) were completing unpaid outdoor housework, such as mowing lawns and painting fences. Approximately one-quarter (n = 10, 26%) were involved in recreational activities, including bushwalking, camping, cycling, or attending an outdoor party. Most people (n = 31, 82%) reported consuming daily news media, mainly through television and the internet. Only 12 (32%) were able to recall a health warning about heatwaves or hot weather in the days before the incident that led to their presentation to the ED. In response to our final open-ended question inviting interviewees to share any other information about their health or behaviour during hot weather, some volunteered information expressing surprise or embarrassment that they had developed heat-illness, indicated that they had underestimated the heat, or told that they would not usually have acted in the way they had (see Supplementary Table 2, doi.org/10.6084/m9.figshare.24558397).
Table 3. Line list of heat exposure for 38 detailed survey responses
| Age band, years | Sex | Time, hoursa | Setting | Activity | Detail of heat exposure |
| 35–64 | Female | 0.5 | Outdooor | Walking | Walked home from train station |
| 17–34 | Male | 4 | Outdoor | Working | Landscaping |
| 35–64 | Male | 4 | Indoor | Working | Sales work |
| 35–64 | Male | 8 | Indoor | Working | Warehouse work |
| 65+ | Male | 2 | Outdoor | Housework | Doing yard work – mowing and cleaning |
| 17–34 | Male | 8 | Indoor | Working | Job in open warehouse |
| 5–16 | Female | 2 | Indoor | Shopping | Shopping indoor |
| 35–64 | Female | 0.5 | Outdoor | Recreation | Golf |
| 5–16 | Female | 1 | Outdoor | Recreation | Swimming |
| 35–64 | Male | 2 | Outdoor | Working | Working and going out |
| 35–64 | Female | 2 | Outdoor | Recreation | Bushwalking |
| 17–34 | Female | 8 | Indoor | Working | In restaurant on floor duty; no air conditioning |
| 5–16 | Male | 1 | Indoor | Recreation | School physical education |
| 65+ | Male | 2 | Indoor | Recreation | Golf – sitting or standing at range |
| 35–64 | Male | 3.5 | Indoor | Recreation | Function club – air conditioning not working |
| 35–64 | Male | 2 | Outdoor | Recreation | Training run, 30 kilometres |
| 17–34 | Female | 0.5 | Indoor | Shopping | Walking in shopping centre |
| 35–64 | Female | 1 | Indoor | Recreation | Waiting to get a table at restaurant |
| 65+ | Female | 10 | Outdoor | Recreation | Got lost when out for a walk |
| 65+ | Female | 2 | Indoor | Recreation | Club; air conditioning not working |
| 5–16 | Female | 1 | Outdoor | Recreation | In spa |
| 35–64 | Male | 6 | Outdoor | Housework | Painting tar |
| 65+ | Male | 2 | Outdoor | Housework | Mowing lawn |
| 35–64 | Female | 2.5 | Outdoor | Housework | Gardening |
| 65+ | Female | 3.5 | Outdoor | Shopping | Walking |
| 17–34 | Male | 11 | Outdoor | Working | Building work |
| 35–64 | Male | 2.5 | Outdoor | Working | Moving items |
| 17–34 | Male | 2 | Outdoor | Working | Fell asleep in the car after loading trucks |
| 35–64 | Female | 2.5 | Indoor | Other | Sitting on veranda |
| 65+ | Male | 0.5 | Outdoor | Shopping | Returning from shops |
| 35–64 | Female | 72 | Outdoor | Recreation | Returning from camping trip |
| 65+ | Female | 4 | Outdoor | Recreation | Walked from hospital into town centre and return |
| 35–64 | Male | 6 | Outdoor | Housework | Moving house – lifting boxes and furniture |
| 35–64 | Female | 2 | Outdoor | Recreation | 15 kms bicycle ride |
| 65+ | Male | 2.5 | Outdoor | Recreation | Party in backyard – standing and sitting |
| 65+ | Male | 24 | Indoor | Indoor | Does not like air conditioning |
| 17–34 | Male | 2 | Outdoor | Working | Putting up scaffolding |
| 17–34 | Male | 96 | Outdoor | Working | Military exercises |
a Time spent on heat exposure activity.
Discussion
Our study aimed to pilot a surveillance system to provide information about environmental, personal, and behavioural risk factors or vulnerabilities to heat. We obtained detailed information about risk from nearly one-third of people who presented to EDs with ‘heat problems’. In the subsample of interviewees, we found a mainly healthy working-age and middle-aged group exposed to heat through either work, recreational activity or activity around the home, with most exposed to heat outdoors. There were more male than female emergency presentations – our interviewed subsample suggests this likely reflects more outdoor work.
A low response rate limited our study. In the first summer, there was a long time lag between the presentation to ED and the attempted interview, which probably contributed to the poor response rate. The response rate improved to a small extent when we obtained data from PHREDSS weekly in 2018/19 and attempted interviews much closer to the time of the ED presentation. There were other indicators that our interview sample was biased: interviewees were slightly older, more likely to be female, and were predominantly English-speaking. Our study was also limited by the persons identified by the diagnostic codes for ‘heat problems’. The ‘heat problems’ codes are found within the external injury subset of codes. Persons are given these diagnostic labels when they have a clear history of heat exposure. Older cohorts with chronic conditions without a history of outdoor heat exposure were not captured. It is possible that older people and people with chronic conditions were not captured because they were protected in their homes. However, we know from time series studies that older cohorts with chronic conditions contribute importantly to the excess morbidity and mortality observed during heat waves and that it affects a wide range of medical conditions beyond those immediately coded to heat.20 For example, during the 2017/18 and 2018/19 summer periods, there were 820 presentations for dehydration to EDs in Western Sydney. Within that group, there may be further unidentified presentations with heat illness.
In the group we interviewed, there was some evidence that people underestimated personal risk from heat exposure. This group should have had opportunities to hear and see heat warnings and modify their plans and activities. For example, during the summer of 2018/19, NSW Health published five heat warning media releases that focused on signs of heat-related illness, precautions to take, and populations considered particularly vulnerable. A review of media sources showed multiple media releases and articles in online and television news sources disseminating this information. Most of the group interviewed engaged with media daily, yet only one-third could recall hearing messaging around heat waves.
Previous studies have identified that warning systems are less likely to reach those with less education, older adults and those with low income.21 Our study identified a group that underestimates their individual risk, making them more likely to engage in behaviours and activities that may lead to heat-related illness.
We were strongly interested in the relevant features of the home and the surrounding built environment that may make people more vulnerable to heat. We were surprised that we identified so few individuals exposed to heat in their home environment. Severe heat waves may be necessary to uncover deficiencies in our homes and environments. The French heatwave of August 2003 resulted in nearly 15 000 excess deaths.2 Death was associated with manual occupation; not leaving home; reduced mobility; pre-existing cardiovascular, mental health and neurological conditions; having a bedroom directly under the roof and an increase in local small area temperature index. Dressing lightly and using a cooling device or technique was protective.2 In a 1995 Chicago heatwave, similar associations were found between death and living conditions, such as living on the top floor, under a flat roof, and in an apartment, while access to a working air conditioner, an air-conditioned lobby or visiting a cooling shelter was protective.3 In the US, building characteristics (at a state level) shown to be linked to heat-related morbidity and mortality include building age, prevalence of air conditioning and thermal properties of external walls and roof. Building materials, ventilation and shading devices are crucial to reduce indoor temperatures.13 A working air conditioner is a significant protective factor against heat-related illness.4,11 However, there are concerns about the affordability of air conditioning for the most vulnerable, access for people who rent, reliability in times of power outages and environmental cost.12
There is now a strategic commitment to mitigate and increase heat resilience in our homes and built environments in high-level NSW strategic plans.22 There is a recognition of the importance of a multiagency approach to mitigating and adapting to heat, particularly in Western Sydney.23 Since 2004, new housing in NSW must comply with the Building and Sustainability Index (BASIX), which prescribes targets for thermal comfort for annual heating loads. However, there is a recognition that BASIX will be inadequate in a warming climate.24
Several technical barriers need to be overcome to implement a system of active follow-up surveillance for heat illness through EDs. To improve the representativeness of the cohort with heat illness, it is necessary to access a broader group of people than the small group presenting with ‘heat problems’. This requires a modified surveillance case definition, which will need to undergo testing and validation. The time and resource cost of individual interviews is a challenge. A sampling approach or more automated questionnaire generation may be needed to make surveillance feasible within resources. The response rate may be improved if there is a timely interview and/or an automated questionnaire within a few days of presentation.
Our study is just one example of an approach to improving our understanding of risk factors for heat-related illness. To implement this active surveillance approach would require investment and commitment. Other complementary approaches would also contribute to our knowledge, including survey methods and real-time data collection during heatwaves. Adopting a more comprehensive and regular reporting of morbidity and mortality associated with heat illness and innovative approaches to surveillance for risk factors have not been high priorities in health but are timely as the climate changes. The call for better reporting of heat-health outcomes and risks often comes from organisations external to health.23,25 Health data is critical to demonstrate the cost-benefit of investment across infrastructure, housing and other sectors.
Conclusion
In this study of individuals presenting to Western Sydney EDs with ‘heat problems’ in two consecutive summers, we found an active middle-aged or working-age cohort with a clear history of heat exposure, mainly outdoors. This group was reasonably aware of the risk of heat illness, but some individuals underestimated this risk. Specific messaging and communication strategies may be needed to reach this group.
To extend an understanding of heat illness risk factors in the home and built environment and to identify those who could benefit from home intervention, a broader, more representative group of people presenting with ‘heat-illness’ will need to be identified. Constructing a modified definition of heat illness to capture this group seems a worthwhile goal but will require careful testing and validation.
Finally, if we are to adapt to the growing threat of increasing frequency, duration, and intensity of heat events due to climate change, we need better data to understand the interaction between personal factors, home and neighbourhood environments and behaviour. With modification, surveillance methods could enhance our understanding of risk and contribute to the evidence base to support changes to protect those at risk.
Acknowledgements
We would like to acknowledge the PHREDSS team in NSW Health for providing data and advice.
This paper is part of a special issue of the journal focusing on urban planning and development for health, which has been produced in partnership with the Healthy Populations and Environments Platform (formerly the Healthy Urban Environments Collaboratory), within Maridulu Budyari Gumal (the Sydney Partnership for Health, Education, Research and Enterprise, SPHERE).
Peer review and provenance
Externally peer reviewed, invited.
Copyright:
© 2023 Conaty S, et al. This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International Licence, which allows others to redistribute, adapt and share this work non-commercially provided they attribute the work and any adapted version of it is distributed under the same Creative Commons licence terms.
References
- 1. Kilbourne EM, Choi K, Jones TS, Thacker SB. Risk factors for heatstroke. A case-control study. JAMA. 1982;247(24):3332–6. CrossRef | PubMed
- 2. Vandentorren S, Bretin P, Zeghnoun A, Mandereau-Bruno L, Croisier A, Cochet C, et al. August 2003 heat wave in France: risk factors for death of elderly people living at home. Eur J Public Health. 2006;16(6):583–91. CrossRef | PubMed
- 3. Semenza JC, Rubin CH, Falter KH, Selanikio JD, Flanders WD, Howe HL, et al. Heat-related deaths during the July 1995 heat wave in Chicago. N Engl J Med. 1996;335(2):84–90. CrossRef | PubMed
- 4. Zhang Y, Nitschke M, Krackowizer A, Dear K, Pisaniello D, Weinstein P, et al. Risk factors of direct heat-related hospital admissions during the 2009 heatwave in Adelaide, Australia: a matched case-control study. BMJ Open. 2016;6(6):e010666. CrossRef | PubMed
- 5. Bobb JF, Obermeyer Z, Wang Y, Dominici F. Cause-specific risk of hospital admission related to extreme heat in older adults. JAMA. 2014;312(24):2659–67. CrossRef | PubMed
- 6. Basu R, Pearson D, Malig B, Broadwin R, Green R. The effect of high ambient temperature on emergency room visits. Epidemiology. 2012;23(6):813–20. CrossRef | PubMed
- 7. Xu Z, FitzGerald G, Guo Y, Jalaludin B, Tong S. Assessing heatwave impacts on cause-specific emergency department visits in urban and rural communities of Queensland, Australia. Environ Res. 2019;168:414–9. CrossRef | PubMed
- 8. Thompson R, Hornigold R, Page L, Waite T. Associations between high ambient temperatures and heat waves with mental health outcomes: a systematic review. Public Health. 2018;161:171–91. CrossRef | PubMed
- 9. Hansen A, Nitschke M, Saniotis A, Benson J, Tan Y, Smyth V, et al. Extreme heat and cultural and linguistic minorities in Australia: perceptions of stakeholders. BMC Public Health. 2014;14:550. CrossRef | PubMed
- 10. Ebi KL, Capon A, Berry P, Broderick C, de Dear R, Havenith G, et al. Hot weather and heat extremes: health risks. Lancet. 2021;398(10301):698–708. CrossRef | PubMed
- 11. Naughton MP, Henderson A, Mirabelli MC, Kaiser R, Wilhelm JL, Kieszak SM, et al. Heat-related mortality during a 1999 heat wave in Chicago. Am J Prev Med. 2002;22(4):221–7. CrossRef | PubMed
- 12. Jay O, Capon A, Berry P, Broderick C, de Dear R, Havenith G, et al. Reducing the health effects of hot weather and heat extremes: from personal cooling strategies to green cities. Lancet. 2021;398(10301):709–24. CrossRef | PubMed
- 13. Hu M, Zhang K, Nguyen QC, Tasdizen T, Krusche KU. A multistate study on housing factors influential to heat-related Illness in the United States. Int J Environ Res Public Health. 2022;19(23):15762. CrossRef | PubMed
- 14. Wilson LA, Morgan GG, Hanigan IC, Johnston FH, Abu-Rayya H, Broome R, et al. The impact of heat on mortality and morbidity in the Greater Metropolitan Sydney Region: a case crossover analysis. Environ Health. 2013;12:98. CrossRef | PubMed
- 15. Muscatello DJ, Churches T, Kaldor J, Zheng W, Chiu C, Correll P, et al. An automated, broad-based, near real-time public health surveillance system using presentations to hospital Emergency Departments in New South Wales, Australia. BMC Public Health. 2005;5:141. CrossRef | PubMed
- 16. Agency ADH. SNOWMED CT-AU and Australian Medicines Terminology May 2022 Release. Canberra; Australian Government, Australian Digital Health Agency; 2022 [cited 2023 Oct 3]. Available from:www.digitalhealth.gov.au/newsroom/product-releases/snomed-ct-au-and-australian-medicines-terminology-may-2022-release
- 17. Katz S, Downs TD, Cash HR, Grotz RC. Progress in development of the index of ADL. Gerontologist. 1970;10(1):20–30. CrossRef | PubMed
- 18. Kliem S, Mossle T, Rehbein F, Hellmann DF, Zenger M, Brahler E. A brief form of the Perceived Social Support Questionnaire (F-SozU) was developed, validated, and standardized. J Clin Epidemiol. 2015;68(5):551–62. CrossRef | PubMed
- 19. Microsoft Corporation. Microsoft Excel. Microsoft; 2023 [cited 2023 Nov 6]. Available from: microsoft.com/en-au/microsoft-365
- 20. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP.; 2013 [cited 2023 Nov 6]. Available from: stata.com
- 21. Kim M, Kim, H, You, M. The role of public awareness in health protective behaviours to reduce heatwave risk. Meteorological Applications. 2014;21(4):867–72. CrossRef
- 22. Office of Energy and Climate Change. NSW climate change adaption strategy. NSW; Adapt NSW, NSW Government; 2022 [cited 2023 Jul 19]. Available from: www.climatechange.environment.nsw.gov.au/about-adaptnsw/nsw-climate-change-adaptation-strategy
- 23. Western Sydney Regional Organisation of Councils. Turn down the heat: strategy and action plan. Sydney: WSROC; 2018 [cited 2023 Oct 28]. Available from: www.wsroc.com.au/projects/project-turn-down-the-heat
- 24. Western Sydney Regional Organisation of Councils. Future proofing residential development in Western Sydney. Sydney; WSROC; 2022. [cited 2023 Oct 8]. Available from: www.wsroc.com.au/projects/project-turn-down-the-heat/future-proofing-residential-development
- 25. Natural Hazards Research Australia. Research priorities: national research priorities for disaster risk reduction and community resilience to the impacts of natural hazards. Victoria; Natural Hazards Research Australia; 2021 [cited 2023 Oct 29]. Available from: www.naturalhazards.com.au/sites/default/files/2022-01/Research%20Priorities%20Discussion%20Paper%20Final%2006102021.pdf


