Abstract
Objective: This manuscript describes the novel approach to developing a toolkit to support meaningful consumer involvement in clinical trials in Australia to help guide others in considering the development of similar resources.The toolkit aims to support greater consumer involvement in shaping how clinical research is prioritised, designed and conducted.
Type of program or service: A working group of researchers, research organisations and consumers was established to co-develop the Consumer Involvement and Engagement Toolkit (the ‘Toolkit’), a digital resource to guide researchers and organisations regarding consumer involvement in clinical trials.
Findings: A literature review and international scan of best practice revealed numerous resources outlining best practice for consumer involvement in clinical research and clear evidence of its impact and value. Through a novel content-sharing process, we were able to utilise these resources to develop a comprehensive Toolkit for researchers and research organisations that provides world-class guidance.
Lessons learnt: There is a growing movement to ensure consumer involvement in healthcare, including in clinical research. We discovered its proponents were willing to share their tools and resources to promote international consumer involvement. Although these international tools and resources needed adaptation to suit the Australian research environment, this was achievable with far less effort than developing them from scratch.
Full text
Introduction
Consumer involvement in health system operations is a common theme across many international initiatives to improve clinical research conduct.1-3 The Australian Government Department of Health is implementing the National Clinical Trials Governance Framework, which extends the National Safety and Quality Health Service ‘Partnering with Consumers’ accreditation standard to clinical trials.4 This requires healthcare organisations to develop, implement, and maintain systems to ensure consumers and their communities guide all aspects of clinical research strategy. However, many commentators caution that for effective and meaningful consumer involvement, organisations and their researchers must see the value of this activity, be skilled and funded to undertake it, and ensure the consumers they involve have the confidence and support to contribute fully and effectively.5-7
In 2018, two government-funded organisations, the Australian Clinical Trials Alliance (ACTA) and Clinical Trials: Impact & Quality (CT:IQ), surveyed clinical trial networks,coordinating centres and industry to determine the extent and impact of consumer involvement in their trials.8 The surveys confirmed that additional support for researchers, research organisations and consumers would strengthen consumer involvement practices across the sector, both at an organisational and trial level.8 In response, ACTA and CT:IQ began work in October 2018 to develop a comprehensive online resource, which was launched in October 2019.
This paper describes the rapid development of the Consumer Involvement & Engagement Toolkit (the ‘Toolkit’) and the novel approach to content sharing that has enabled the developers to produce a comprehensive national resource within a tight project timeframe.
Methods
A working group of researchers, research organisations and consumers was established to codevelop the Toolkit. Individuals were identified through an open call to ACTA member organisations. Their first task was to develop the Toolkit’s project plan and its core design and development parameters. The key requirements identified are summarised in Table 1.
Table 1. Stakeholder advice to guide the Toolkit’s design and development
| Requirements | Rationale |
| Conduct a literature search of international best practice and partner with international organisations to enable sharing of resources and ideas. | To build on existing resources and enrich the Toolkit’s content, accelerate its development and minimise its development cost. |
| Use the literature to support Toolkit content so that researchers/organisations can access the evidence underpinning its content. | To ensure the Toolkit content is informed by current thinking and evidence of best practice. |
| Include sections on equity and diversity and provide translations for any consumer-facing content that reflects the Australian population’s diversity. | To support ethical research and to make research more generalisable to the Australian population. To ensure the Toolkit’s content is accessible. |
| Include practical tools, forms, and templates suitable for use in all health disciplines, that can be downloaded for use (and amended to reflect local processes and the specifics of the involvement activity). | To ensure researchers and organisations do not have to duplicate efforts by defining and developing these tools themselves. |
The Working Group favoured a digital resource (website) that could be readily updated as consumer involvement best practices evolve. To ensure the Toolkit was populated with evidence-informed practice, a synthesis of international guidance and published literature was undertaken to identify best practices for consumer involvement. This review included:
A Medline database search using key words including ‘patient’, ‘public’, ‘consumer’, ‘involvement’, ‘engagement’, ‘health’, ‘research’ and ‘value’ among others, identified 1344 articles (published from 2005 to 2021) of which 103 were relevant. A snowball search of the 6 systematic reviews from this search and a Google Scholar search identified a further 48 articles. A total of 157 publications qualified for review.
An appraisal of guidance provided by key international bodies responsible for consumer and community involvement, including National Institute for Health and Care Research (NIHR) Involve (UK)9, the Strategy for Patient-Oriented Research (Canada)3, the Clinical Trials Transformation Initiative (US)10, and the Patient-Centered Outcomes Research Institute (US).11
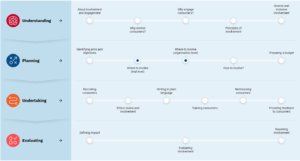
The review also informed the choice of topic headings for the Toolkit’s ‘Routemap’, a series of 19 nodes positioned in a sequence that prepares researchers to conduct consumer involvement, before illustrating how it can be operationalised across the life cycle of a clinical trial (Figure 1).12
Since consumer involvement consists of discrete activities along the clinical trial life cycle (involvement activities can take place at any stage during a trial), the Toolkit’s design was modelled on the UK’s Clinical Trials Toolkit13 offering ‘a dip in and dip out’ approach to information access (Figure 1). Each node hyperlinks to a landing page that provides a detailed description of the topic, signposts to external resources including publications from the review to support best-practice, and downloadable tools to help researchers operationalise their consumer and community involvement activities.
Figure 1. Consumer involvement and engagement route map concept (click figure to enlarge)
Source: Australian Clinical Trials Alliance. Consumer Involvement & Engagement Toolkit.12
Upon establishment of the core design, a priority-setting workshop was held with a wider group of stakeholders utilising a ‘dotmocracy’ voting approach (in which participants vote on their chosen options using a limited number of dot stickers) to ratify further and inform content development to meet user needs. Content writing progressed in parallel with the website build to meet international standards for web-content accessibility.14 Following an iterative review and revision process, the Toolkit was finalised in September 2019.
This project was conducted in fulfilment of ACTA’s project plan as agreed by the Department of Health rather than as a research study, therefore ethics approval was not sought.
Results
The Toolkit guides researchers and organisations (both not-for-profit and commercial), covering four key consumer involvement stages: 1) understanding, 2) planning, 3) undertaking and 4) evaluating activities (Figure 1). As described above, the content displayed within each node opens a landing page that describes a key area of activity and provides tools to help operationalise consumer involvement. Examples include:
- A template to develop a local consumer involvement strategy
- A confidentiality agreement and Terms of Reference document for advisory groups
- Recruitment tips
- Consumer involvement agreements
- A costing tool so researchers can budget for their involvement activities
- Templates for researchers to evaluate their involvement activities.
Users can adapt these tools to add organisation logos and amend them to align with local processes or the specifics of their involvement activity. A small but growing section of the Toolkit is dedicated to supporting consumers seeking to get involved in clinical trials. We have developed videos to enhance awareness of clinical research in several languages to ensure they are accessible to Australia’s multicultural population. We illustrate consumer involvement with a series of case studies. We include a ’Consumer Involvement Pack’ to improve consumers’ understanding of the trial process and introduce new consumer representatives to their role in clinical trials.
Discussion
While the Toolkit now serves as a consolidated resource to support consumer involvement in research, its development had its challenges. Firstly, there was a lack of standardisation in the terminology used to describe the activity. The terms ‘involvement’ and ‘engagement’ and ‘participation’ are used interchangeably in Australia and internationally. The Working Group recommended alignment with prominent national guidance on involving consumers in research15, and so the following definitions were adopted:
- Involvement: Where consumers and community representatives actively work with researchers and research organisations to help shape decisions about health research priorities, policy, and practice.
- Engagement: Where information and knowledge about research are shared with consumers and the community so that they are better informed on why, how, where and by whom research is conducted.
- Participation: Where patients or healthy volunteers take part in clinical trials.
The original plan for the Toolkit was to signpost users to existing national and international resources. However, very few could be adopted without alteration due to the local or regional initiatives, infrastructure, and terminology embedded within them. We generated a simple reciprocal content sharing arrangement to overcome this issue that enabled parties to adapt resources with appropriate acknowledgement. Each time an exemplar document or tool was identified, the authors and corresponding organisations were contacted, and without exception those approached agreed to the sharing arrangement to further the consumer involvement movement internationally.
As local research groups were also encouraged to share their tools during the Toolkit’s development, the project’s leadership team quickly recognised that a transparent method for triaging new content was needed. This was managed by appointing the Working Group (with no vested interests) as the final arbiter. When multiple versions of similar tools were received, the Group was free to select a single tool for adaptation and acknowledgement or to suggest the content from several tools be combined to create a new resource, with contributors acknowledged.
Considering the scale of this project, the timeframe for its delivery was ambitious (12 months from concept to launch). Success in delivering the project on time was due in no small part to the codesign approach taken and the commitment of all involved. The funders’ initial concern that involving consumers in every decision would cause delays proved unfounded, as consumers unambiguous articulation of ‘end-user needs’ served to reduce indecision on the part of other team members.
Further work
Future plans for the Toolkit include an evaluation of its use and value to stakeholders and enhancements that were not addressed in the first phase of development, such as:
- Plain-language training and resources for both researchers and consumers
- A mechanism for more diverse involvement of consumers and communities
- A platform to connect researchers and consumers
- Resources to promote consumer-driven research including opportunities for patients and their communities to generate research ideas and proposals.
As some stakeholders are yet to be convinced that consumer involvement justifies the resources used and the costs incurred, work to build the value proposition for consumer involvement is needed. International guidelines for reporting the context, process, and impact of consumer involvement are now available16. As the reporting of consumer involvement in research manuscripts increases, the Toolkit will continue to highlight its value.
Conclusion
Consumer involvement is a critical component of good research practice and Australian Government plans to improve the quality and safety of clinical trials. But the broader uptake of consumer involvement in research is likely to depend on efforts to debunk the common misconception that consumer involvement is simply when researchers communicate with consumers to enrol them in their trials. It is not.
By delineating common terms such as involvement, engagement, and participation, equipping researchers with knowledge of why, where, and how to involve consumers, and the tools to do so, the Toolkit now supports the embedding of meaningful consumer involvement in Australian clinical research.
Many valuable resources for consumer involvement exist internationally, and to avoid reinventing the wheel, the project used a novel content sharing agreement to enable the inclusion of international resources (e.g., tools and templates) to support consumer involvement in Australia. Drawing on the experience and expertise of international advocates of consumer involvement has enriched the Toolkit and enabled the development of a national asset. This would not have been feasible within the project’s timeframe and budget without this approach. We promote the Toolkit to facilitate broader sector engagement in the practice of consumer involvement here in Australia and as a resource to be shared and adapted for use further afield.
Acknowledgements
This project received grant funding from the Australian Government. TS received fees from ACTA for consultancy work on the Toolkit but was not paid for any aspect of this manuscript development. JB has received consultancy fees from ACTA unrelated to the Toolkit project, and consultancy fees from various medical research institutes and a trial network. MS has received payment for advisory and education consultancy from Bard BD unrelated to the Toolkit project. RM has received consultancy fees from Lilly and Metavention and speaking fees from Lilly, Boehringer-Ingleheim and Sanofi unrelated to the Toolkit project.
Peer review and provenance
Externally peer reviewed, not commissioned.
Copyright:
© 2022 Symons et al. This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International Licence, which allows others to redistribute, adapt and share this work non-commercially provided they attribute the work and any adapted version of it is distributed under the same Creative Commons licence terms.
References
- 1. Hunter NL, O’Callaghan KM, Califf RM. Engaging patients across the spectrum of medical product development: view from the US Food and Drug Administration. JAMA. 2015;314(23):2499–500. CrossRef | PubMed
- 2. Staniszewska S, Denegri S, Matthews R, Minogue V. Reviewing progress in public involvement in NIHR research: developing and implementing a new vision for the future. BMJ Open. 2018;8(7):e017124. CrossRef | PubMed
- 3. Canadian Institutes of Health Research. Canada's strategy for patient-oriented research. Canada; CIHR: 2021 [cited 2021 Dec 12]. Available from: cihr-irsc.gc.ca/e/41204.html
- 4. Australian Commission on Safety and Quality in Health Care: National Clinical Trials Governance Framework. Sydney: ACSQHC; 2020 [cited 2021 Dec 12]. Available from: www.safetyandquality.gov.au/standards/clinical-trials
- 5. Wright D, Foster C, Amir Z, Elliott J, Wilson R. Critical appraisal guidelines for assessing the quality and impact of user involvement in research. Health Expect. 2010;13(4):359–68. CrossRef | PubMed
- 6. Telford R, Boote JD, Cooper CL. What does it mean to involve consumers successfully in NHS research? A consensus study. Health Expect. 2004;7(3):209–20. CrossRef | PubMed
- 7. Boote J, Barber R, Cooper C. Principles and indicators of successful consumer involvement in NHS research: Results of a Delphi study and subgroup analysis. Health Policy. 2006:75(3):280–97. CrossRef | PubMed
- 8. Australian Clinical Trials Alliance. Consumer involvement consultation report. Melbourne: ACTA; 2018 [cited 2021 Dec 12]. Available from: clinicaltrialsalliance.org.au/resource/acta-consumer-involvement-consultation-report-2/
- 9. National Institute of Health Research (NIHR): Involve.UK: NIHR; 2022 [cited 2022, May 17]. Available from www.nihr.ac.uk/documents/ppi-patient-and-public-involvement-resources-for-applicants-to-nihr-research-programmes/23437
- 10. Clinical Trials Transformation Initiative. Durham NC: CTTI; 2022 [cited 2022 May 17]. Available from: ctti-clinicaltrials.org/
- 11. Patient-Centred Outcomes Research Institute (PCORI). Washington DC: PCORI; 2022 [cited 2022 May 17]. Available from: www.pcori.org/
- 12. Australian Clinical Trials Alliance. Toolkit for researchers and research organisations. Melbourne: ACTA; 2019 [cited 2022 May 17]. Available from: involvementtoolkit.clinicaltrialsalliance.org.au/toolkit
- 13. National Institute of Health Research Clinical Trials Toolkit. Routemap. Southampton, UK: NIHR; 2022 [cited 2021 Dec 12]. Available from: www.ct-toolkit.ac.uk/routemap/
- 14. Web Content Accessibility Guidelines. WCAG 2 Overview. Cambridge, MA: WAI; 2018 [cited 2021 Dec 12]. Available from: www.w3.org/WAI/standards-guidelines/wcag/
- 15. National Health and Medical Research Council and Consumers Health Forum of Australia. Statement on consumer and community involvement in health and medical research. Canberra: NHMRC & CHF; 2016 [cited 2022 Apr 22]. Available from: www.nhmrc.gov.au/about-us/publications/statement-consumer-and-community-involvement-health-and-medical-research
- 16. Staniszewska S, Brett J, Simera I, Seers K, Mockford C, Goodlad S et al. GRIPP2 reporting checklists: tools to improve reporting of patient and public involvement in research. BMJ. 2017;358:J3453. CrossRef | PubMed