Abstract
Objectives: To review the most recent population-based estimates of keratinocyte cancer incidence in Australia, to describe the trends over time and to calculate lifetime risk of developing these skin cancers.
Methods: We conducted a literature search of PubMed/MEDLINE from 2001 to August 2021 to identify relevant literature. We defined eligible articles as those reporting population-based studies of adults and excluded studies that reported only on high-risk or paediatric populations, or on incidence of precursor or related lesions. We summarised identified studies qualitatively. We calculated lifetime risk of developing keratinocyte cancer using the methods of Cancer Research UK, adjusting for multiple primaries and the competing risk of death.
Results: We identified six eligible studies. In the absence of compulsory notifications of keratinocyte cancer to state and territory cancer registries in Australia, all estimates of national incidence rates of basal cell carcinoma (BCC) and squamous cell carcinoma (SCC) have limitations. The most recent population-based estimates of people annually affected for the period 2011–2014 (BCC: 770/100 000 person years; SCC: 271/100 000 person years) represent the lower end of the possible range of incidence rates nationally. Because many people are affected by multiple lesions, the lesion-based incidence estimates are more than double the person-based rates (BCC: 1565/100 000 person years; SCC: 580/100 000 person years). Analyses of temporal trends in treatment rates (excisions, cryotherapy/curettage) show increases over time, most marked for people aged 55 years or older. We estimate that 69% of Australians will have at least one excision for histologically confirmed keratinocyte cancer in their lifetime (60% to age 79 years).
Conclusion: The available evidence on national incidence rates is out of date and of moderate quality, but indicates very high rates of keratinocyte cancer in Australia. We recommend that population-based cancer registries work towards statutory notification and routine reporting of keratinocyte cancer in Australia.
Full text
Introduction
Australia is colloquially known as the skin cancer capital of the world, with skin cancer often referred to as ‘our national cancer’.1 High-quality and up-to-date information on skin cancer incidence is needed to inform healthcare planning, to identify priority high-risk groups that might be targeted for specific prevention activities, and to gauge the impact of skin cancer prevention campaigns.
Reporting of diagnoses of melanoma and Merkel cell carcinoma to cancer registries of all states and territories in Australia is mandated by law, enabling monitoring of trends over time and across subgroups of the population.2-4 In contrast, the most common skin cancers, basal cell carcinoma (BCC) and squamous cell carcinoma (SCC), collectively referred to as keratinocyte cancer, are not registered by state and territory cancer registries except in Tasmania, despite causing substantial morbidity and treatment costs.5 As a result, contemporary incidence statistics are not routinely available.
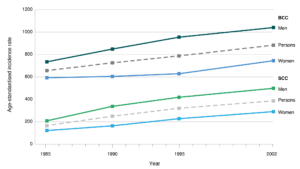
Estimates of keratinocyte cancer incidence have therefore relied on ad hoc surveys or treatment records of geographically defined populations6,7 or administrative data from the Medicare Benefits Schedule (MBS), a listing of the Medicare services subsidised by the Australian Government.8 Population-based surveys conducted between 1985 and 2002 indicated increases in incidence (Figure 1)9-13; however, there has been no national population-based incidence survey since 2002. More recent estimates of incidence are based on MBS data.14-16 The item codes used by Medicare to reimburse claims for excision of histologically confirmed keratinocyte cancer have shown very high concordance with histopathologic diagnoses (approximately 97% concordance).17 However, many keratinocyte cancers are treated destructively, without histological confirmation, and thus all estimates based only on pathology records underestimate the true incidence.
Our aims were to describe the most recently published population-based estimates of the incidence of keratinocyte cancer in Australian adults nationally or within defined geographic regions (both person based and tumour based); to describe the temporal trends, including age- and sex-specific trends over time; and to calculate lifetime risk.
Figure 1. Age-standardised incidence rates (per 100 000) for basal cell carcinoma and squamous cell carcinoma from national surveys conducted in 1985, 1990, 1995 and 2002 (click to enlarge)
BCC = basal cell carcinoma; SCC = squamous cell carcinoma
Note: Rates are standardised to the 1960 world population
Sources: National Cancer Control Initiative Skin Cancer Working Group12, Staples et al.13
Methods
Systematic review
We followed the PRISMA guidelines for reporting the systematic review.18
Data sources and searches
We conducted a literature search of PubMed/MEDLINE (Bethesda, MD, US: US National Library of Medicine) from January 2001 to August 2021 to identify relevant literature on the incidence of invasive keratinocyte cancer in Australia. We used the following subject heading terms or text words: incidence, skin neoplasms, basal, BCC, cutaneous squamous, SCC, non-melanoma, keratinocyte cancer, Australia, Queensland, New South Wales, Victoria, Northern Territory, South Australia, Tasmania and Western Australia (Appendix 1: Search terms, available from: figshare.com/articles/journal_contribution/Appendix_1_-_search_terms_docx/19159718). We read the titles and abstracts of all identified studies and excluded those that were not relevant; the full texts of the remaining articles were read to determine if they met the inclusion criteria. We hand-searched the reference lists of retrieved articles to identify other eligible studies.
Study selection and data extraction
We included articles that reported on population-based studies of adults (18+ years). We excluded studies that reported solely on high-risk populations (e.g. transplant recipients), paediatric populations, or incidence of precursor or related lesions (specifically intra-epidermal carcinoma or keratoacanthoma). Where multiple reports described the same population, we included the most recent or most comprehensive report (i.e. covering the longest time period or the largest population).
One investigator (CO) abstracted data from identified studies (checked by a second investigator, NP). The following information was recorded for each study: design, location, years of data collection, source and definition of the study cohort, incidence statistics reported (keratinocyte cancer, BCC, SCC) and annual percentage change in rates over time. Potential sources of bias were also recorded. We conducted a qualitative synthesis of the identified studies.
Lifetime risk
We used the methods of Cancer Research UK to calculate lifetime risk of developing keratinocyte cancer using the ‘adjusted for multiple primaries’ (AMP) method, which is conservative and accounts for competing risk of mortality and the occurrence of multiple primaries.19,20 We obtained the age- and sex-specific counts of people with one or more excision claims for histologically confirmed BCC and SCC from the Medicare 10% sample21 for the year 2014 using the methods described by Pandeya et al.16 We obtained data on all-cause mortality and estimated resident population for 2014 from the Australian Institute of Health and Welfare (AIHW).22 We calculated deaths from keratinocyte cancer in 2014 by subtracting melanoma (ICD-10 C43) deaths from deaths from skin cancer (ICD-10 C43, C44) using the AIHW General Record of Incidence of Mortality (GRIM) database 2018.23,24
Results
Our literature search identified 290 articles, of which six were eligible for inclusion in our review (Table 1; see Appendix 2, available from: figshare.com/articles/journal_contribution/Appendix_2_-_PRISMA_flow_diagram/19160081).13-16,25,26 One study reported on the most recent national incidence survey13, two used aggregated data from Medicare14,15, two used individual-level Medicare data16,25, and the final study reported cancer registry data for a single state (Tasmania).26
Table 1. Characteristics of the six included studies
| Authors (year) | Geographic region | Years of data collection | Study population/cohort | Outcomes |
| Staples et al. (2006)13 | Australia | 1989–2004 | 57 215 Australians aged 14+ years randomly selected from the electoral roll | Keratinocyte cancer incidence BCC incidence SCC incidence |
| Fransen et al. (2012)14 | Australia | 1997–2010 | Aggregated Medicare data | Treatment rates for keratinocyte cancer |
| Olsen et al. (2014)15 | Australia | 2000–2011 | Aggregated Medicare data | Treatment rates for keratinocyte cancer |
| Pandeya et al. (2017)16 | Australia | 2011–2014 | Individual-level Medicare data | Treatment rates for keratinocyte cancer, BCC and SCC |
| Adelson et al. (2018)25 | South Australia | 2010–2014 | Individual-level Medicare data | Treatment rates for keratinocyte cancer |
| Ragaini et al. (2021)26 | Tasmania | 1978–2018 | Cancer registry data | Keratinocyte cancer incidence BCC incidence SCC incidence |
BCC = basal cell carcinoma; SCC = squamous cell carcinoma
Incidence/incidence trends
National survey
The most recent national survey of skin cancer incidence in Australia was conducted in 2002.13 It conducted face-to-face interviews with 57 215 Australians aged 14 years or older from addresses selected at random from the Australian electoral roll, of whom 817 (1.4%) were confirmed as having one or more diagnoses of skin cancer in the past year. The age-standardised (Australian standard population 2001) person-based incidence rate for the year 2002 was 1288/100 000 for BCC and 593/100 000 for SCC (1719/100 000 for keratinocyte cancer; Table 2). Incidence of keratinocyte cancer was higher among men than women (44% higher for BCC and 75% higher for SCC; Table 2) and was highest among people aged 70 years or older compared with younger age groups. Between the surveys conducted in 1985 and 2002, incidence of BCC increased only among people aged 60 years or older, and incidence of SCC increased only among people aged 50 years or older.
Table 2. Age-standardised incidence of keratinocyte cancer (Australian 2001 population) in Australia
| Authors (year of publication) | Year(s) | Persons or lesions | Age standardised incidence rate per 100 000 | ||
| Men | Women | People | |||
| National-level studies | |||||
| Staples et al. (2006)13 | |||||
| BCC | 2002 | Persons | 1541 | 1070 | 1288 |
| SCC | 2002 | Persons | 772 | 442 | 593 |
| Keratinocyte cancer | 2002 | Persons | 2051 | 1436 | 1719 |
| Fransen et al. (2012)14 | |||||
| Keratinocyte cancera | 2010 | Lesions | 3174 | ||
| Olsen et al. (2014)15 | |||||
| Surgical excisionb | 2011 | Lesions | 2448 | ||
| Cryotherapy/curettagec | 2011 | Lesions | 895 | ||
| Pandeya et al. (2017)16 | |||||
| BCC | 2011–2014 | Persons | 899 | 656 | 770 |
| SCC | 2011–2014 | Persons | 341 | 209 | 271 |
| Keratinocyte cancerd | 2011–2014 | Persons | 1824 | 1272 | 1531 |
| BCC | 2011–2014 | Lesions | 2027 | 1149 | 1565 |
| SCC | 2011–2014 | Lesions | 800 | 381 | 580 |
| Keratinocyte cancerd | 2011–2014 | Lesions | 4158 | 2250 | 3154 |
| State-level studies | |||||
| South Australia: Adelson et al. (2018)25 | |||||
| Keratinocyte cancer | 2010–2014 | Persons | 1467 | ||
| Tasmania: Ragaini et al. (2021)26 | |||||
| First incidence | |||||
| BCC | 2018 | Persons | 363 | ||
| SCC | 2018 | Persons | 249 | ||
| Annual incidence | |||||
| BCC | 2018 | Persons | 891 | ||
| SCC | 2018 | Persons | 514 | ||
BCC = basal cell carcinoma; SCC = squamous cell carcinoma
a Medicare Benefits Schedule (MBS) item claims for treatment of keratinocyte cancer by excision, curettage, laser or liquid nitrogen cryotherapy (includes surgical treatment for recurrent lesions)
b MBS item claims for surgical excision of primary BCC or SCC
c MBS item claims for cryotherapy/curettage of malignant lesions
d Includes item codes for excision of BCC/SCC that are claimed for intra-epidermal carcinomas and keratoacanthomas
Aggregated Medicare data
Two studies used aggregated Medicare data to estimate keratinocyte cancer treatment rates; these two studies reported on number of treatment procedures per 100 000 population rather than number of people affected.14,15 Fransen and colleagues examined the rate of services to treat skin cancer (by excision, curettage, laser or liquid nitrogen cryotherapy) between 1997 and 2010, noting an 36% increase in the number of treatments over that period, from 2338/100 000 to 3174/100 000 (Table 2). The increase was only apparent for those aged 55 years or over.14 Similarly, Olsen and colleagues examined data on excisions for histologically confirmed keratinocyte cancer for the period 2000–2011 inclusive, and reported average annual increases in excisions for confirmed keratinocyte cancer of 2.2% for women and 3.3% for men overall.15 In 2011, the treatment rates were 2448/100 000 for excision of a primary BCC or SCC and 895/100 000 for cryotherapy/serial curettage of a malignant lesion (Table 2). Significant increases in both excisions and treatment with cryotherapy/serial curettage over time were observed only among people aged 55 years or older; declines were observed for those aged younger than 55 years.15 This occurred despite significant increases in diagnostic biopsy procedures between 2000 and 2011 across all age groups.
Individual-level Medicare data
Because aggregated administrative claims data cannot account for multiplicity, Pandeya and colleagues used individual-level Medicare data from a 10% sample21 of the MBS database covering the period 2011–2014 to calculate both person- and lesion-based rates of excisions for primary keratinocyte cancer.16 Because MBS item codes for keratinocyte cancer excision do not discriminate between BCC and SCC, data on the BCC:SCC ratio within strata of age and sex observed from a large prospective cohort study in the state of Queensland (QSkin)27 were used to apportion the incidence due to BCC and SCC. The age-standardised (Australian standard 2001) person-based excision rates for BCC and SCC were lower than the incidence rates reported from the national survey in 2002, at 770 and 271/100 000, respectively. An apparent discrepancy arises between the estimated rate for total keratinocyte cancer and the rate for BCC and SCC in the Medicare analysis because it is estimated that 32% of all billing claims using the item codes for keratinocyte cancer excision relate to other neoplastic skin lesions, including keratoacanthoma and intra-epidermal carcinoma, and thus only about 68% of total claims are for histologically confirmed BCC or SCC.28 In the study by Pandeya and colleagues16, multiplicity was common, with 2.7% of Australians aged 20 years or over diagnosed with more than one keratinocyte cancer in the 4-year period to 2014 (47% of those affected had more than one excision); the lesion-based excision rates were 1565/100 000 for BCC and 580/100 000 for SCC (Table 2). The excision rates were higher among men than women (37% higher for BCC and 63% higher for SCC), and men were more likely than women to undergo multiple excision procedures. Queensland had the highest excision rates (person based: 1355/100 000 for BCC and 467/100 000 for SCC), and Victoria and Tasmania (combined) the lowest (person based: 482/100 000 for BCC and 175/100 000 for SCC).21
A second study used individual-level Medicare data for the state of South Australia.25 MBS item codes for initial excision of primary BCC or SCC, together with those for Mohs surgery and cryotherapy/serial curettage for a confirmed malignant lesion, were used to identify cases, although the majority of claims (90%) were for initial surgical excision. The age-standardised (Australian standard 2001) annual rate of treatment for at least one histologically confirmed keratinocyte cancer over the period 2010–2015 was 1467/100 000 people (Table 2). The number of treatment claims for keratinocyte cancer increased between 2010 and 2015 by 59%.
Tasmanian Cancer Registry
The study using cancer registry data for the population of the state of Tasmania26 reported on both first and annual incidence of BCC and SCC; both measures were person based. For incidence of first BCC and SCC, only the first notification over the period 1985–2018 was counted in people with no prior notification, since registration began in 1978; for annual incidence, only one notification of BCC and SCC per person was counted for each year. In 2018, the age-standardised (Australian standard 2001) incidence of first BCC and SCC was 363/100 000 and 249/100 000, respectively; incidence increased on average by 3% per year for BCC and 4% per year for SCC over the period 1985–2018.26 In 2018, the age-standardised (Australian standard 2001) annual incidence was 891/100 000 for BCC and 514/100 000 for SCC (Table 2). Annual incidence of BCC and SCC also increased over the period 1978–2018, on average by 5% per year for BCC and 6% per year for SCC, although the rates appeared to stabilise from 2014. Incidence was higher among men than among women, and among older than among younger age groups; incidence of first BCC and SCC was highest in the 80–84 age group and the 85 or over age group, respectively, and increases were observed across all age groups between 1985 and 2018.
Lifetime risk, and risk to age 79 years
We estimated that the lifetime risk of having at least one excision for a histologically confirmed keratinocyte cancer in 2014 was 69% (73% for men and 65% for women) (Table 3). The risk to age 79 years was 60% (65% for men and 53% for women).
Table 3. Cumulative and lifetime risk of having one or more excisions for histologically confirmed keratinocyte cancer in Australia, 2014
| Age, years | Risk | ||
| Men | Women | People | |
| 65–69 | 44.4 | 34.2 | 39.6 |
| 70–74 | 55.8 | 43.8 | 50.5 |
| 75–79 | 64.5 | 52.7 | 59.5 |
| 80–84 | 69.6 | 59.2 | 65.4 |
| Lifetimea | 72.5 | 64.6 | 69.4 |
a Lifetime risk is not ‘average lifetime’, but includes all people in the population
Discussion
We have reviewed the published data on population-based estimates of incidence of keratinocyte cancer in Australia and calculated lifetime risk using the latest available population-based national incidence data. A previous review published in 2015 included studies published between 1948 and 2011 and was not limited to population-based studies.7
Until 2002, periodic national surveys provided the only data on the burden of keratinocyte cancer on the Australian population. These population-based surveys confirmed self-reported diagnoses of skin cancer in the previous 12 months in only around 60% of cases through contact with treating doctors. The rates were adjusted to account for unconfirmed reports by multiplying the rates by a factor of 1.64 in the case of the 2002 survey13, corresponding to a confirmation rate of 61%. This may have led to an overestimation of BCC and SCC person-based incidence. On the other hand, people with multiple BCCs or SCCs were counted once only for each type of keratinocyte cancer; given that around 25% of people with either BCC or SCC had multiple tumours, this would have led to underestimation of the total keratinocyte cancer burden treated annually. A further limitation of the national incidence surveys is the known unreliability of self-reported history of keratinocyte cancer, and the likelihood of underreporting.29
The more recent estimates of national incidence of BCC and SCC from the analysis of individual-level Medicare data for the period 2011–2014 by Pandeya et al.16 were lower than annual incidence rates for the state of Tasmania for the year 2018.26 The person-based BCC:SCC ratio also differed between the two studies (1.7 for Tasmania vs 2.8 for the national data). The lower BCC:SCC ratio for Tasmania is unexpected, based on other work12, and underscores the need for more population-based data to fully understand the distributions of BCC and SCC across all parts of Australia.
Other limitations must be considered when interpreting the findings of these two studies. Neither study accounted for lesions treated destructively and without histological confirmation. On the other hand, the incidence rates from the Tasmanian Cancer Registry26 may be overestimates because the automated coding system could not discriminate between biopsies and excisions of the same lesion, which may have resulted in some BCCs and SCCs being counted twice (i.e. from a report of a biopsy and an excision). However, a sensitivity analysis excluding notifications within 3 months of the index case resulted in only slightly lower incidence rates. The analyses by Pandeya et al.16 did not include the item code for biopsies, a proportion of which may be keratinocyte cancer, which could lead to an underestimate of the incidence of BCC and SCC. The observation from QSkin that up to 32% of Medicare claims for keratinocyte cancer excisions may not be for BCC or SCC may also only apply to Queensland.
Our estimate of the lifetime risk of having at least one excision for a histologically confirmed keratinocyte cancer in 2014 is 69% (73% for men and 65% for women). This is not directly comparable to the previous reports because they used different methods. An advantage of our calculations of lifetime risk was the ability to account for the occurrence of multiple primaries, and to adjust for the competing risk of mortality.19 However, a limitation was the inability to account for lesions treated destructively. Using data from the 2002 national survey, Staples et al.13 estimated that the cumulative risk of at least one keratinocyte cancer by age 70 years was 70% for men and 58% for women. Ragaini et al.26 reported that the cumulative risk of keratinocyte cancer in Tasmania to age 80 years was 42% for men and 35% for women; the estimates were only slightly attenuated using the AMP method.
An important finding of our review was that all recent reports of national incidence of BCC and SCC in the Australian population have limitations. The reported person-based excision rates of 770/100 000 for BCC and 271/100 000 for SCC16 are likely to represent the lower end of the possible range of incidence rates nationally. Moreover, many people are affected by multiple lesions, and the lesion-based rates are at least twice as high as the person-based rates. What appears more certain is that the incidence of keratinocyte cancer in Australia has increased during the past three decades, at a rate of around 2–6% per year, mostly affecting older age groups. Some data suggest differences by age, with declines seen over time in younger age groups but increases among those who are in their sixth decade or older. The decline among younger people may reflect both the success of primary prevention campaigns that began in the 1980s (and were therefore most likely to benefit recent birth cohorts) and demographic changes (i.e. an increased proportion of the population of non-European ancestry and thus at lower inherent risk of skin cancer). Increasing incidence among older Australians likely reflects higher levels of cumulative exposure to ultraviolet radiation experienced by older birth cohorts.
Conclusion
We estimate that 69% of Australians will have at least one excision for keratinocyte cancer in their lifetime, and this is likely to increase as the population ages. This high and increasing burden of skin cancer emphasises the need for continued investment in skin cancer education and prevention. Measures include support for national mass-media campaigns about the need for sun protection to prevent sunburn and skin cancer (use of clothing, hats, sunscreen and sunglasses), implementation of additional regulatory measures to protect children and workers from the harms of overexposure to sunlight (primary and secondary schools, workplaces), and the provision of shade in public and spectator settings.
Reliable estimates of disease incidence are fundamentally important to inform prevention activities, to monitor their success, and to plan for future healthcare services. We recommend that population-based cancer registries consider working towards statutory notification and routine reporting of keratinocyte cancer in Australia. Synoptic reporting by pathologists would facilitate automated data abstraction and coding to this end.
Acknowledgements
This work was supported by the National Health and Medical Research Council (NHMRC) (grant number APP1185416). DW is supported by a Research Fellowship (APP1155413) from the NHMRC. BR is employed by the Tasmanian Cancer Registry.
This manuscript is part of a special issue focusing on skin cancer prevention. The special issue was supported by and developed in partnership with Cancer Council, and also supported by the Australian Radiation Protection and Nuclear Safety Agency, the Australasian College of Dermatologists and the Australian Skin and Skin Cancer Research Centre.
Peer review and provenance
Externally peer reviewed, invited.
Copyright:
© 2022 Olsen et al. This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International Licence, which allows others to redistribute, adapt and share this work non-commercially provided they attribute the work and any adapted version of it is distributed under the same Creative Commons licence terms.
References
- 1. House of Representatives Standing Committee on Health. Skin cancer in Australia: our national cancer. Report on the Inquiry into Skin Cancer in Australia. Canberra: Parliament of the Commonwealth of Australia; 2015 [cited 2022 Jan 19]. Available from www.aph.gov.au/Parliamentary_Business/Committees/House/Health/Skin_Cancer/Report
- 2. Whiteman DC, Green AC, Olsen CM. The growing burden of invasive melanoma: projections of incidence rates and numbers of new cases in six susceptible populations through 2031. J Invest Dermatol. 2016;136(6):1161–71. CrossRef | PubMed
- 3. Olsen CM, Thompson JF, Pandeya N, Whiteman DC. Evaluation of sex-specific incidence of melanoma. JAMA Dermatol. 2020;156(5):1–8. CrossRef | PubMed
- 4. Olsen CM, Pandeya N, Whiteman DC. International increases in Merkel cell carcinoma incidence rates between 1997 and 2016. J Invest Dermatol. 2021;141(11):2596–01. CrossRef | PubMed
- 5. Gordon LG, Elliott TM, Olsen CM, Pandeya N, Whiteman DC. Multiplicity of skin cancers in Queensland and their cost burden to government and patients. Aust N Z J Public Health. 2018;42(1):86–91. CrossRef | PubMed
- 6. Green A, Battistutta D, Hart V, Leslie D, Weedon D. Skin cancer in a subtropical Australian population: incidence and lack of association with occupation. The Nambour Study Group. Am J Epidemiol. 1996;144(11):1034–40. CrossRef | PubMed
- 7. Perera E, Gnaneswaran N, Staines C, Win AK, Sinclair R. Incidence and prevalence of non-melanoma skin cancer in Australia: a systematic review. Australas J Dermatol. 2015;56(4):258–67. CrossRef | PubMed
- 8. Australian Government Department of Health. Medical Benefits Schedule. Canberra: Australian Government; 2022 [cited 2022 Jan 19]. Available from: www.mbsonline.gov.au
- 9. Giles GG, Marks R, Foley P. Incidence of non-melanocytic skin cancer treated in Australia. Br Med J (Clin Res Ed). 1988;296(6614):13–17. CrossRef | PubMed
- 10. Marks R, Staples M, Giles GG. Trends in non-melanocytic skin cancer treated in Australia: the second national survey. Int J Cancer. 1993;53(4):585–90. CrossRef | PubMed
- 11. Staples M, Marks R, Giles G. Trends in the incidence of non-melanocytic skin cancer (NMSC) treated in Australia 1985–1995: are primary prevention programs starting to have an effect? Int J Cancer. 1998;78(2):144–8. CrossRef | PubMed
- 12. National Cancer Control Initiative Skin Cancer Working Group. The 2002 national non-melanoma skin cancer survey. Melbourne: NCCI; 2003 [cited 2021 Jan 19]. Available from: www.canceraustralia.gov.au/sites/default/files/publications/nmscreport1_504af01fd661f.pdf
- 13. Staples MP, Elwood M, Burton RC, Williams JL, Marks R, Giles GG. Non-melanoma skin cancer in Australia: the 2002 national survey and trends since 1985. Med J Aust. 2006;184(1):6–10. CrossRef | PubMed
- 14. Fransen M, Karahalios A, Sharma N, English DR, Giles GG, Sinclair RD. Non-melanoma skin cancer in Australia. Med J Aust. 2012;197(10):565–8. CrossRef | PubMed
- 15. Olsen CM, Williams PF, Whiteman DC. Turning the tide? Changes in treatment rates for keratinocyte cancers in Australia 2000 through 2011. J Am Acad Dermatol. 2014;71(1):21–6.e1. CrossRef | PubMed
- 16. Pandeya N, Olsen CM, Whiteman DC. The incidence and multiplicity rates of keratinocyte cancers in Australia. Med J Aust. 2017;207(8):339–43. CrossRef | PubMed
- 17. Thompson BS, Olsen CM, Subramaniam P, Neale RE, Whiteman DC. Medicare claims data reliably identify treatments for basal cell carcinoma and squamous cell carcinoma: a prospective cohort study. Aust N Z J Public Health. 2016;40(2):154–8. CrossRef | PubMed
- 18. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–12. CrossRef | PubMed
- 19. Sasieni PD, Shelton J, Ormiston-Smith N, Thomson CS, Silcocks PB. What is the lifetime risk of developing cancer?: the effect of adjusting for multiple primaries. Br J Cancer. 2011;105(3):460–5. CrossRef | PubMed
- 20. Ahmad AS, Ormiston-Smith N, Sasieni PD. Trends in the lifetime risk of developing cancer in Great Britain: comparison of risk for those born from 1930 to 1960. Br J Cancer. 2015;112(5):943–7. CrossRef | PubMed
- 21. Medicare Australia. Linkable de-identified 10% sample of Medicare Benefits Schedule (MBS) and Pharmaceutical Benefits Schedule (PBS) Australia. Canberra: Medicare Australia; 2016 [cited 2017 Jul]. researchdata.ands.org.au/linkablede-identified-schedule-pbs/673945 (URL no longer active)
- 22. Australian Institute of Health and Welfare. General Record of Incidence of Mortality (GRIM) books 2018: all causes combined. Canberra, Australia: AIHW; 2020 [cited 2022 Jan 19]. Available from www.aihw.gov.au/reports/life-expectancy-deaths/grim-books/contents/data-visualisation
- 23. Australian Institute of Health and Welfare. General Record of Incidence of Mortality (GRIM) books 2018: melanoma of the skin. Canberra, Australia: AIHW; 2020 [cited 2022 Jan 19]. Available from www.aihw.gov.au/reports/life-expectancy-deaths/grim-books/contents/data-visualisation
- 24. Australian Institute of Health and Welfare. General Record of Incidence of Mortality (GRIM) books 2019: melanoma of the skin. Canberra, Australia: AIHW; 2020 [cited 2022 Jan 19]. Available from: www.aihw.gov.au/reports/life-expectancy-deaths/grim-books/contents/grim-excel-workbooks
- 25. Adelson P, Sharplin GR, Roder DM, Eckert M. Keratinocyte cancers in South Australia: incidence, geographical variability and service trends. Aust N Z J Public Health. 2018;42(4):329–33. CrossRef | PubMed
- 26. Ragaini BS, Blizzard L, Newman L, Stokes B, Albion T, Venn A. Temporal trends in the incidence rates of keratinocyte carcinomas from 1978 to 2018 in Tasmania, Australia: a population-based study. Discov Oncol. 2021;12(30). CrossRef
- 27. Olsen CM, Green AC, Neale RE, Webb PM, Cicero RA, Jackman LM et al. Cohort profile: the QSkin Sun and Health Study. Int J Epidemiol. 2012;41(4):929–i. CrossRef | PubMed
- 28. Thompson BS, Pandeya N, Olsen CM, Dusingize JC, Green AC, Neale RE, Whiteman DC. Keratinocyte cancer excisions in Australia: who performs them and associated costs. Australas J Dermatol. 2019;60(4):294–300. CrossRef | PubMed
- 29. FitzGerald K, Stephens N, Newman L, Venn A. Inaccuracies in self-reported histories of non-melanoma skin cancer. Aust N Z J Public Health. 2007;31(1):87. CrossRef | PubMed